Towards Universal Health Coverage | 12 Dec 2024
This editorial is based on “Whither universal health coverage in India?” which was published in The Financial Express on 12/12/2024. The article brings into picture the challenges in India's journey towards Universal Health Coverage (UHC), highlighting limited insurance coverage (41% households) and poor quality of public healthcare. It emphasizes the need to reduce inequalities, improve services, and ensure equitable health outcomes nationwide.
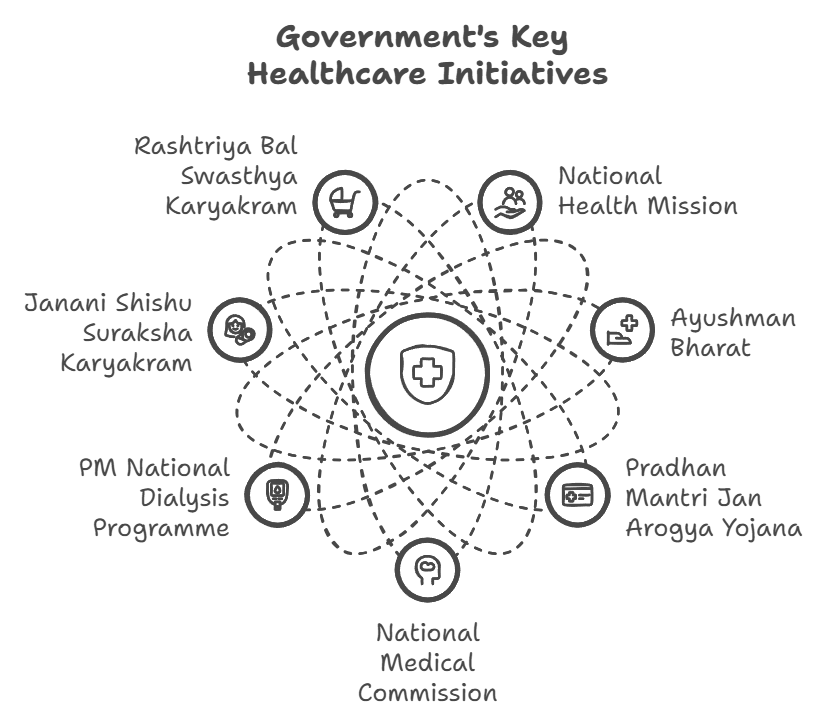
For Prelims: Universal Health Coverage, Medical tourism, Economic Survey 2023-24, Ayushman Bharat Scheme, Out-of-Pocket Expenditure, Fit India Movement, Poshan Abhiyaan, Ayushman Arogya Mandir, National Health Policy, 2017., Ayushman Bharat Digital Mission, Aadhaar, Non-communicable diseases, Viability Gap Funding.
For Mains: Current Status of India's Healthcare Sector, Issues Hindering Universal Health Coverage in India.
India's journey towards Universal Health Coverage (UHC) has been marked by significant challenges and incremental progress. Despite implementing various health schemes since 1948, only 41% of Indian households have health insurance, and half avoid government health facilities due to poor care quality. The path to true universal health coverage demands a focused approach that prioritizes reducing inequalities, improving service quality, and achieving consistent health outcomes across all socioeconomic groups and regions.
What is the Current Status of India's Healthcare Sector?
- About: The Healthcare Sector reached a valuation of US$ 372 billion in 2023, employing 7.5 million people, with significant growth in telemedicine, health-tech, and medical tourism.
- India's hospital market, valued at US$ 98.98 billion in 2023, is projected to double by 2032.
- The telemedicine market is set to grow to US$ 5.4 billion by 2025, while the e-health market may hit US$ 10.6 billion in the same period.
- Doctor-Population Ratio and Medical Tourism: India's doctor-to-population ratio stands at 1:854, including both allopathic and AYUSH practitioners.
- Additionally, medical tourism has positioned India as a global hub, contributing US$ 7.69 billion in 2024, and projected to grow to US$ 14.31 billion by 2029.
- Foreign Investment: Foreign investments in drugs and pharmaceuticals reached US$ 22.57 billion by March 2024, signaling robust growth and global confidence in India's healthcare ecosystem.
What are the Issues Hindering Universal Health Coverage in India?
- Inadequate Public Health Expenditure and Weak Primary Healthcare System: Despite being the world's most populous country, India spends only 1.9% of its GDP on healthcare (Economic Survey 2023-24)
- India's healthcare pyramid is inverted, with an over-reliance on tertiary care and neglect of primary health systems.
- Diseases like diabetes and hypertension, which can be managed at the primary level through early screening and intervention, often go undiagnosed until complications arise, pushing patients to tertiary care.
- In states like Uttar Pradesh and Bihar, the absence of robust screening programs at the primary level exacerbates this issue.
- India's healthcare pyramid is inverted, with an over-reliance on tertiary care and neglect of primary health systems.
- Regional Disparities in Healthcare Access: Healthcare infrastructure is unevenly distributed, with urban areas enjoying better facilities than rural ones.
- For example, while 70% of India’s healthcare professionals are concentrated in urban regions, 65% of the population resides in rural areas.
- A recent Rural Health Statistics, highlights significant shortfalls in rural CHCs, with over 80% gaps in surgeons, physicians, pediatricians, and around 75% in obstetricians and gynecologists.
- High Burden of Non-Communicable Diseases: India is witnessing a rapid transition to NCDs, which now account for 65-66% of total deaths (WHO, 2022).
- Diseases like diabetes, cardiovascular disorders, and cancers strain the healthcare system, which is still focused on communicable diseases.
- Factors such as pollution, poor sanitation, and malnutrition exacerbate health inequalities.
- Air pollution alone caused 1.67 million deaths in India in 2019. Furthermore, 40% of rural households lack access to safe drinking water, increasing vulnerability to diseases like cholera and typhoid.
- Inefficiencies in Implementation of Government Schemes: Flagship schemes like Ayushman Bharat aim to provide health coverage to 50 crore citizens, yet their reach is hampered by poor awareness and uneven implementation.
- According to a recent CAG report, almost 7.5 lakh people in the Ayushman Bharat Scheme’s beneficiary database were linked with a single cell phone number.
- The report also said that patients earlier shown as “dead” continued to avail treatment under the scheme.
- The maximum number of such cases were in Chhattisgarh, Haryana, Jharkhand, Kerala and Madhya Pradesh.
- Poor Health Insurance Penetration: India's 95% population remain uninsured, 73% lack health coverage.
- The unorganized sector and informal workers, who form 90% of the workforce, remain excluded from employer-based insurance.
- As a result, high Out-of-Pocket Expenditure on health is impoverishing some 55 million Indians annually, with over 17% households incurring catastrophic levels of health expenditures
- Fragmentation in Healthcare Governance: India’s federal structure often leads to fragmented healthcare policies, with limited coordination between central and state governments.
- For instance, during Covid-19, the lack of a uniform testing policy created confusion and inefficiencies in disease management.
- States with better health governance, like Kerala, outperformed others in managing outbreaks, reflecting disparities in administrative capacity.
- Low Focus on Preventive Healthcare: Preventive measures such as immunization, screening, and lifestyle interventions are underutilized despite their cost-effectiveness.
- India’s full immunization coverage was only 76.4% in 2021 (NFHS-5), leaving millions of children vulnerable to preventable diseases.
- Additionally, the Fit India Movement and Poshan Abhiyaan face slow implementation, limiting their impact on reducing long-term health burdens.
- Limited Use of Technology and Digital Health: While initiatives like Ayushman Bharat Digital Mission (ABDM) aim to digitize health records, digital penetration remains low in rural areas.
- The absence of standardized data exchange protocols complicates seamless information sharing between different healthcare systems, impeding coordinated patient care and the effective implementation of nationwide health initiatives like the ABDM.
- Dependence on Private Sector: Overburdened public hospitals often divert individuals to seek treatment in the costlier private sector.
- Almost 60% of all hospitalizations, and 70% of out-patient services are delivered by the private sector (NSSO's 75th Round survey on Social Consumption of Health, 2017-18),
- The unregulated nature of private healthcare leads to price gouging and inequitable access, undermining the vision of affordable UHC.
What Measures can be Adopted to Accelerate Universal Health Coverage in India?
- Enhancing Public Health Expenditure and Health Insurance: India must increase its public health spending to at least 2.5% of GDP by 2025, as envisioned in the National Health Policy, 2017.
- This can fund better infrastructure, more healthcare workers, and ensure essential medicines at public facilities.
- Expanding programs like the PM Ayushman Bharat Health Infrastructure Mission, which focuses on creating critical care hospitals in every district, will bridge infrastructure gaps.
- Expanding insurance through targeted schemes will further reduce the financial burden on vulnerable populations.
- India can draw lessons from the Beveridge Model (UK, Nordic countries) by implementing universal healthcare funded through taxation, ensuring equitable access to essential services.
- And also learning from the Bismarck Model (France, Japan), India can adopt a framework of insurance-based healthcare with both employer and employee contributions.
- Strengthening Primary Health Care: Revamping primary health centers (PHCs) and sub-centers with adequate staffing, equipment, and medicines is critical.
- Initiatives like the Ayushman Arogya Mandir under Ayushman Bharat should be expanded with a greater focus on preventive care and management of non-communicable diseases (NCDs).
- For instance, integrating telemedicine services like eSanjeevani with these centers can improve access in rural areas
- Mandatory preventive health screenings for NCDs and other diseases at the PHC level can reduce the long-term disease burden.
- Implementing large-scale health camps, similar to the Rashtriya Swasthya Bima Yojana (RSBY) health drives, can detect issues early, especially in rural and tribal areas.
- Addressing Workforce Shortages: A robust health workforce requires scaling up medical and paramedical education while improving working conditions.
- Expanding the Skill India initiative to include healthcare-specific training for nurses, midwives, and community health workers will address shortages.
- For example, increasing seats in medical colleges and incentivizing rural postings through higher pay and career advancement opportunities can bridge the rural-urban divide.
- Assam introduced financial incentives for doctors in remote regions, setting a replicable precedent.
- Leveraging Digital Health Technology: Accelerating the rollout of the Ayushman Bharat Digital Mission (ABDM) to create a unified digital health ID can streamline patient records and improve healthcare delivery.
- Establishing internet connectivity in rural areas through BharatNet and providing digital training for health workers will ensure inclusivity.
- The integration of telemedicine platforms like Tele-Manas for mental health can further address unmet needs.
- Focus on Preventive Healthcare: Preventive measures such as vaccination, health education, and lifestyle modifications can reduce disease burden and costs.
- Expanding the Poshan Abhiyaan’s scope to address adult malnutrition alongside childhood malnutrition will combat rising non-communicable diseases.
- Strengthening urban sanitation under the Swachh Bharat Mission 2.0 and increasing funding for National Programmes like the NPCDCS (Non-Communicable Diseases Control Program) will have far-reaching impacts.
- Public-Private Partnerships: PPPs can be leveraged for infrastructure development, diagnostics, and tertiary care.
- Schemes like the Viability Gap Funding (VGF) for private hospitals in underserved areas can improve access without excessive costs.
- For example, Rajasthan’s Mukhyamantri Free Medicine Scheme partnered with pharma companies to supply affordable drugs. Expanding similar collaborations can enhance service delivery.
- Reducing Regional Disparities: Central schemes should incentivize states with lower health indices to invest in healthcare infrastructure and workforce development.
- Linking NITI Aayog’s Health Index rankings with performance-based grants under the 15th Finance Commission can motivate lagging states like Bihar and Uttar Pradesh to improve.
- Kerala’s decentralized governance model, which allocates higher budgets to local health institutions, provides a roadmap for success.
- Strengthening Regulatory Mechanisms: Ensuring price control of essential medicines and standardizing treatment costs across private hospitals are critical.
- Expanding the scope of the National Pharmaceutical Pricing Authority (NPPA) and mandating hospitals to display transparent pricing under the Clinical Establishments Act will curb exploitation.
- Price reductions of cardiac stents and knee implants have already saved patients money, showcasing the efficacy of regulation.
- Investing in Research and Indigenous Innovations: India must strengthen research and innovation by funding institutes like ICMR to develop affordable, indigenous healthcare solutions.
- Public health innovations, such as the locally developed Covaxin during Covid-19, demonstrate the potential of self-reliance.
- Establishing regional research hubs can address localized health challenges, such as vector-borne diseases in the Northeast.
- Integrating Traditional Medicine with Modern Healthcare: India’s vast repository of traditional medicine through AYUSH (Ayurveda, Yoga, Unani, Siddha, and Homeopathy) can complement modern healthcare.
- Integrating AYUSH practitioners into the Health and Wellness Centres (HWCs) under Ayushman Bharat can reduce the burden on allopathic practitioners and provide culturally accepted alternatives.
- Comprehensive Mental Health Coverage: Mental health remains underfunded and stigmatized despite rising needs.
- Scaling up the National Mental Health Programme (NMHP) and integrating it with primary healthcare through telemedicine platforms like Tele-Manas can make services accessible.
- Integrating One Health Approach: The One Health approach, which recognizes the interconnectedness of human, animal, and environmental health, is vital for achieving universal health coverage.
- Establish integrated monitoring systems for zoonotic diseases such as Nipah and Avian Influenza, ensuring rapid response mechanisms.
- Expand the scope of the National Centre for Disease Control (NCDC) to collaborate with veterinary and wildlife departments.
Conclusion
While India has made strides in its pursuit of Universal Health Coverage, several significant challenges remain. These include inadequate public health expenditure, regional disparities, poor insurance penetration, and an overburdened healthcare system. To achieve UHC, India must focus on enhancing public health spending, strengthening primary health care, and addressing inefficiencies in government schemes.
|
Drishti Mains Question: "Universal Health Coverage (UHC) is essential for achieving equitable and inclusive development in India." Discuss the challenges in achieving UHC and suggest measures to ensure quality, accessibility, and affordability of healthcare for all. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q“Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)