Governance
Reshaping Inclusive Health Care in India
- 08 Apr 2024
- 19 min read
This editorial is based on “Shaping India’s path to inclusive health care” which was published in The Hindu on 08/04/2024. The article explains how India's health equity issues stem from a complex interplay of factors such as socioeconomic status, education, gender, geography, and access to healthcare services. Addressing these issues requires a multifaceted approach that goes beyond simply improving healthcare facilities.
For Prelims: Universal Health Coverage, Sustainable Development Goals (SDGs), NFHS-5, Pradhan Mantri Jan Arogya Yojana, Right to Health, WHO, Universal Declaration of Human Rights (1948), United Nations, Fundamental Rights, DPSPs, Supreme Court.
For Mains: Challenges in Achieving Universal Health Care/Coverage (UHC), Significance of Healthcare for Viksit Bharat by 2047.
World Health Day, which is observed every year on April 7, unites us around health equity, an essential topic at the heart of global health and justice. The World Health Organization (WHO) has declared health to be a fundamental human right. The theme this year is “My Health, My Right”. There is an alarming gap in health-care access, highlighted by the COVID-19 epidemic, environmental crises, and growing socio-economic gaps.
Even though over 140 nations recognise health as a constitutional right, the WHO Council on the Economics of Health for All reports that more than half the world’s population needs complete access to essential health services. With the passage of World Health Day 2024, it is clear that promoting health equity is a source of optimism for millions of people, going beyond social justice or legislative change.
The United Nations defines inclusive healthcare as “everyone, everywhere should have access to the health services they need without risk of financial hardship.” Sustainable Development Goals (SDGs) target 3.8 (“Achieve universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all”) also focuses on inclusive healthcare.
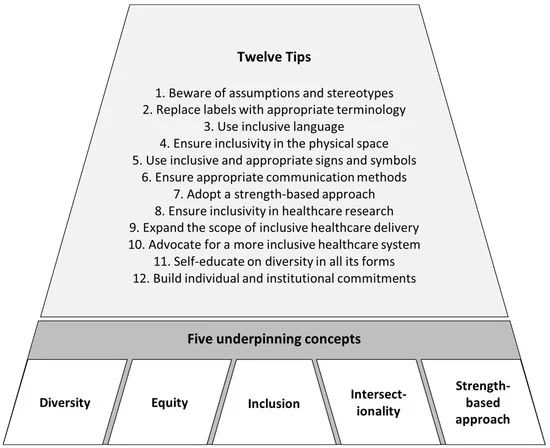
What is Inclusive Healthcare?
There is no one formula that that makes care fully inclusive for everyone. It’s important for inclusive care to be sustainable. That is, everyone involved needs to be willing to revaluate and adapt as necessary. Four hallmarks of inclusive care include:
- Culture of Inclusion:
- Inclusive care should be built into the culture of an organization. All staff—not just those with MDs/MSs, but anyone who interacts with patients—should understand the types of common barriers faced by people.
- Staff should receive regular training to ensure that they do not become yet another challenge for patients to overcome. Inclusive care should begin with the very first interaction with a patient. A sustainable culture of inclusion is not a box to check, but a way of providing the best care for everyone who enters the space.
- Welcoming Spaces:
- Inclusive care has physical spaces that are accessible to people of all abilities. They include materials (clinical and logistical) in the languages spoken by patients. The staff working in inclusive spaces should reflect the same types of diverse groups of people seeking care.
- Accessible Materials:
- Inclusive care extends beyond the physical space occupied to the materials available for patients. Inclusive materials may have large print, be available in multiple languages, use appropriate language (inclusive of all genders and sexual orientations), and be culturally sensitive.
- Valuing All Patients:
- Inclusive care includes patients in the decision-making process and takes patients concerns into account. Whenever possible those providing care should work alongside patients at their educational or intellectual level and with their means and access in mind.
What is the Meaning of Health Equity?
- Every Person Has an Equal Opportunity:
- Health equity ensures that every person has an equal opportunity to achieve their highest health potential, no matter what their circumstances. Recognising that social, economic, and environmental factors impact health outcomes, this idea goes beyond genetics. WHO’s mission is to eliminate unfair and preventable disparities in health among different social and economic categories.
- Addresses the Root Causes:
- True health equity addresses the root causes of health inequities such as poverty, discrimination, limited access to high-quality education, a healthy diet, clean water, fresh air, and housing, and merely grants equal access to health care.
- These differences are made worse by pandemics, climate change, and sociopolitical unrest. India is diverse and has wide socioeconomic gaps. Thus this predicament strikes a chord. Access to health care in rural areas is significantly less than in metropolitan areas. Social and economic barriers exacerbate this disparity.
- True health equity addresses the root causes of health inequities such as poverty, discrimination, limited access to high-quality education, a healthy diet, clean water, fresh air, and housing, and merely grants equal access to health care.
- Adopts a Comprehensive Strategy:
- To guarantee that everyone may live a healthy life, attaining health equity necessitates a comprehensive strategy that goes beyond legislative reform to address the socioeconomic determinants of health. Realising each person’s potential for health demands a concerted effort by governments, communities, and individuals to tear down these obstacles.
What are the Different Challenges to Health Equity?
The road to health equity is fraught with difficulties, ranging from deeply ingrained social injustices to global systemic health concerns, particularly in multicultural countries such as India. Diverse populations need help to get access to high-quality health care in this place.
- The Global Challenges:
- Risks Posed by Pandemics:
- The fight for health equity confronts global challenges that transcend borders and call for collective international action. The COVID-19 pandemic has starkly revealed that infectious diseases target marginalised and vulnerable groups the most, thus widening the health equity gap.
- Climate Change Concerns:
- Climate change poses a serious health risk since it disproportionately impacts low-income and vulnerable people. The health-care provision is severely hampered by conflicts, which destroy infrastructure, uproot communities, and shut off access to vital medical services.
- Risks Posed by Pandemics:
- India-Specific Challenges:
- Large and Diversified Population:
- With a large and diversified population, India faces persistent obstacles to health equity, including notable differences in health-care outcomes and access. Even though access to health care has improved over the past 20 years, there is still much work to be done in rural India.
- According to the 2011 Census, urban slums make up over 17% of India’s metropolitan areas, and exhibit serious health disparities. Health risks are increased by overcrowding, poor sanitation, and restricted access to clean water.
- Infectious diseases, such as tuberculosis, are 1.5 times more common in slums than in non-slum areas, according to the Indian Council of Medical Research (ICMR).
- Disparities Across Caste and Gender:
- Disparities across caste and gender are profound. National Family Health Survey (NFHS)-5 (2019-21) data indicates that Scheduled Castes and Scheduled Tribes experience higher child mortality and lower immunisation rates.
- Additionally, 59% of women in the lowest wealth quintile suffer from anaemia, almost double the rate in the highest quintile, demonstrating the intersection of caste, gender, and economic status in health outcomes.
- Burden of Non-Communicable Diseases:
- Non-communicable diseases (NCDs) account for more than 60% of all fatalities in India. The Public Health Foundation of India points out the necessity for equitable treatment access and preventive health care, stating that the economic effect of NCDs could surpass USD 6 trillion by 2030, which warrants urgent attention by the stakeholders.
- Critical Shortage of Doctors:
- A critical shortage of doctors exacerbates these issues, with WHO data indicating only 0.8 doctors per 1,000 people, which is below the advised ratio. Even though over 75% of health-care professionals work in metropolitan regions, which only account for 27% of the population, the shortage is particularly severe in rural areas.
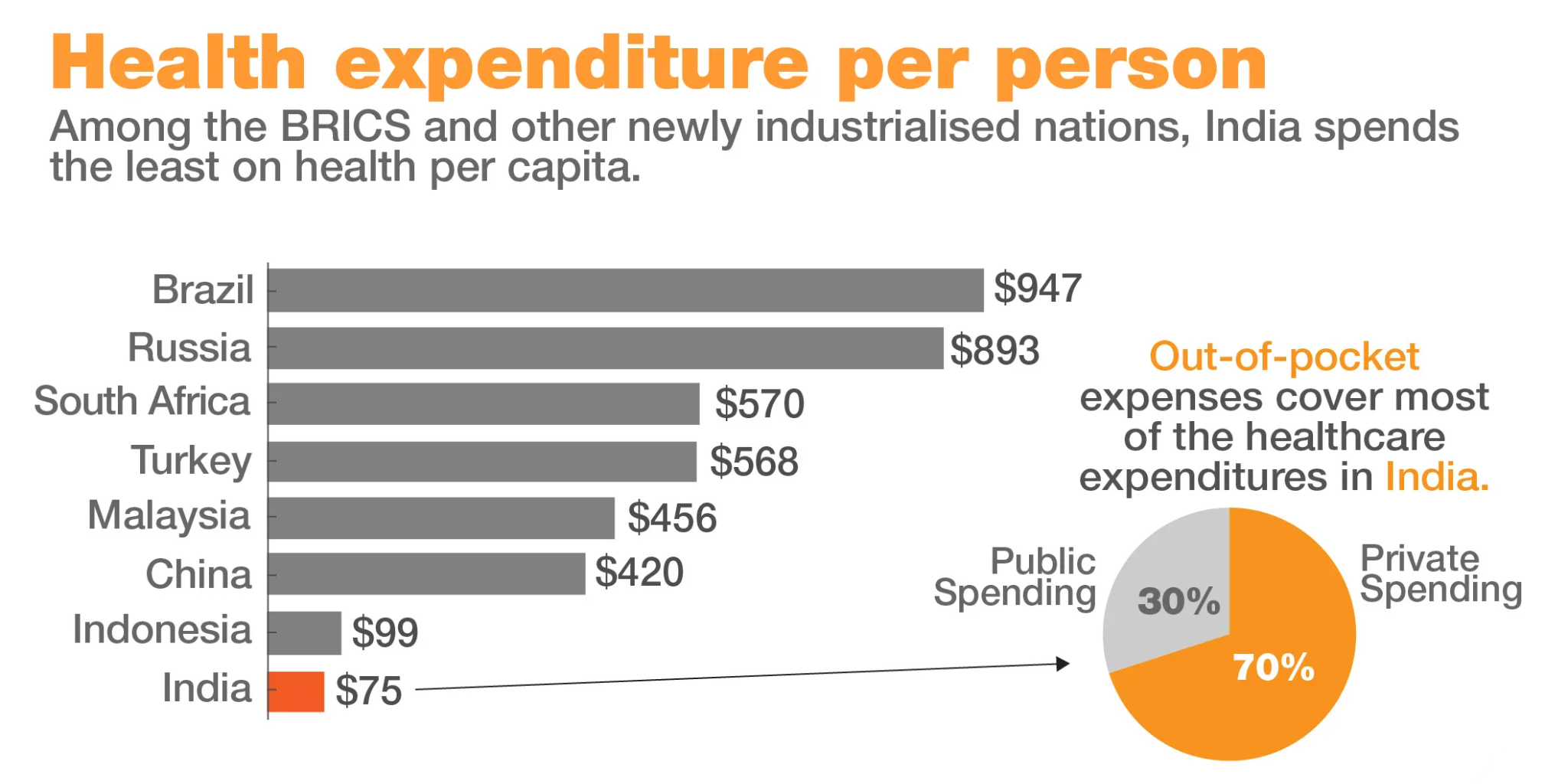
- Lack of Financial Protection:
- Despite the existence of schemes like Janani Shishu Suraksha Karyakram, the average out-of-pocket expenditure per delivery in public health facilities is still high, particularly in urban areas.
- There are significant disparities in out-of-pocket expenditure (OOPE) and access to healthcare services among different states in India. Many north eastern states and larger states have seen a rise in out-of-pocket expenditure between NFHS-4 and NFHS-5.
- The latest report of NFHS-5 revealed that the average out-of-pocket expenditure per delivery in a public health facility is Rs. 2,916, which in the case of urban and rural stands at Rs. 3,385 and Rs. 2,770 simultaneously.
- Large and Diversified Population:
What are the Various Suggestions to be Incorporated in Providing Equitable Healthcare?
- Comprehensive Approach Beyond Healthcare Facilities:
- India’s health equity issues require a comprehensive approach beyond improvements in health-care facilities to address more extensive socioeconomic determinants of health. To move India toward universal health coverage and a more equitable future, the government, civil society, health-care providers, and communities need to work together.
- Achieving health equity requires raising health literacy. India should turn health equality into a shared, community-driven goal by including health education in the National Health Mission (NHM), , enabling its people to seek equitable care and make educated health decisions
- India’s health equity issues require a comprehensive approach beyond improvements in health-care facilities to address more extensive socioeconomic determinants of health. To move India toward universal health coverage and a more equitable future, the government, civil society, health-care providers, and communities need to work together.
- Necessitating Government’s Intervention:
- Governments and officials may influence the state of health through funding, creative policies, and laws. For instance, India’s Ayushman Bharat initiative provides free health coverage to the bottom 40% economically, demonstrating a commitment to reducing health disparities.
- The NHM, which includes both the National Rural Health Mission (NRHM) and the National Urban Health Mission (NUHM), reduces the health-care gap between rural and urban India by expanding access, strengthening infrastructure, and providing essential services to vulnerable populations.
- Governments and officials may influence the state of health through funding, creative policies, and laws. For instance, India’s Ayushman Bharat initiative provides free health coverage to the bottom 40% economically, demonstrating a commitment to reducing health disparities.
- Public and Private Sector Collaboration:
- Together with the government, the public and private health-care sectors provide services to underprivileged communities, emphasising preventive education, workforce development, and infrastructure enhancement.
- Non-governmental organisations and civic societies engage in direct community outreach to draw attention to and resolve regional health concerns. Their collaboration with international and governmental organisations allows them to tailor health initiatives that are culturally sensitive to the community’s unique needs.
- Together with the government, the public and private health-care sectors provide services to underprivileged communities, emphasising preventive education, workforce development, and infrastructure enhancement.
- Reliance on International Institutions:
- International institutions can provide financial and technical resources to support healthcare systems in developing countries. This can help improve infrastructure, training, and access to essential medicines and technologies.
- International institutions such as WHO, the Global Fund for AIDS, Tuberculosis and Malaria, and Gavi-Global Vaccine Alliance support health initiatives in places with limited resources and promote sharing information and resources to enhance health-care systems, especially in countries such as India.
- International institutions can provide financial and technical resources to support healthcare systems in developing countries. This can help improve infrastructure, training, and access to essential medicines and technologies.
- Promoting Innovation and Technical Growth:
- Through innovation and technical growth, particularly in digital health, the commercial sector and charitable organisations advance accessibility and affordability while extending reach and efficacy.
- Research institutes and academic institutions offer crucial insights into health inequalities and the efficacy of interventions, assisting in creating evidence-based practices and policies supported by scientific studies.
- Technological advancements continue to drive innovation in healthcare, leading to improved diagnostics, treatments, and patient care. Some notable advancements include Precision Medicine and Genomics, Artificial Intelligence (AI) and Machine Learning (ML), Wearable Devices and Remote Monitoring and Robotics and Automation.
- Following Organisations With Strong Local Presence:
- Organisations with a strong local presence are essential for health equity. They actively participate in every phase, from planning to evaluation, to guarantee the relevance and effectiveness of health programmes. They also have a thorough understanding of their community’s requirements.
- Adopting Shared Approach and Open Communications:
- Successful collaborations, essential for achieving health equity, depend on open communication, respect for one another, and common goals. They are prepared to adapt to shifting health concerns and community demands because they strongly emphasise empowering communities, sharing knowledge, and building capacity.
- Effective communication across many sectors, ranging from policymakers to grassroots organisations, may significantly enhance health equity and pave the path for a time when access to high-quality health care would be a shared reality rather than a privilege.
- Successful collaborations, essential for achieving health equity, depend on open communication, respect for one another, and common goals. They are prepared to adapt to shifting health concerns and community demands because they strongly emphasise empowering communities, sharing knowledge, and building capacity.
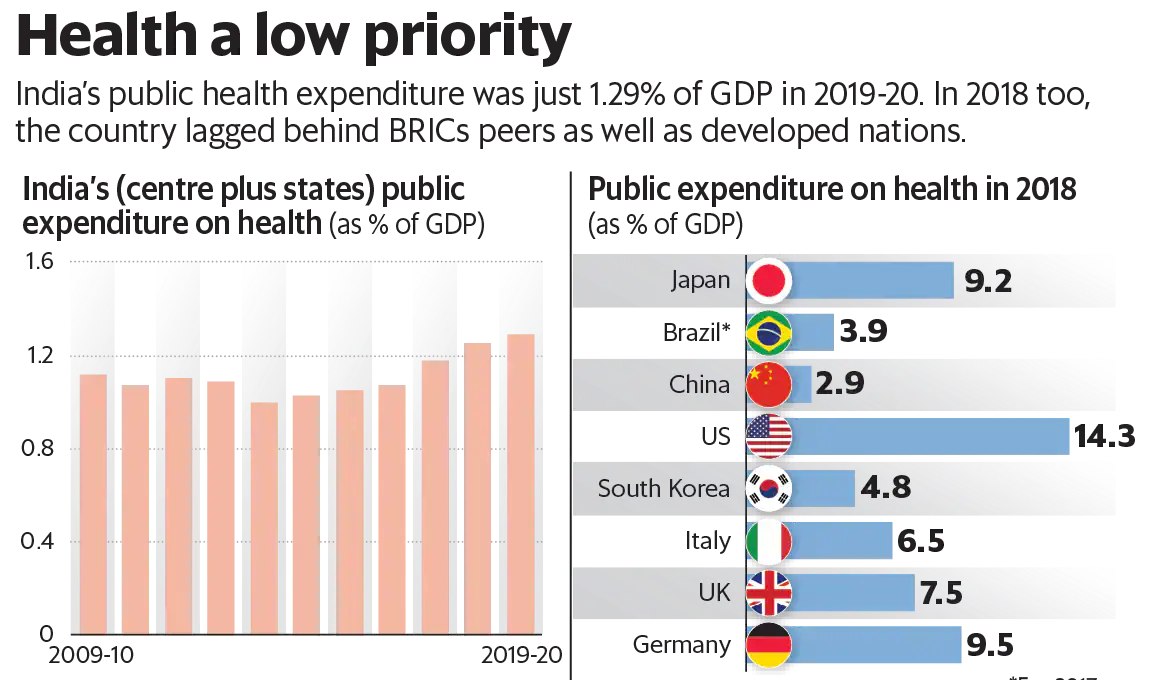
- Increasing Allocation as Percentage of GDP:
- According to the budget estimates for fiscal year 2020, about 1.35% of India's GDP was spent on public health. This was a slight increase compared to the previous fiscal year when about 1.29% of the GDP was spent on healthcare.
- The Fifteenth Finance Commission recommends that the public health expenditure of the Union and States should be increased together to reach 2.5% of GDP (Growth Domestic Product) by 2025.
- Currently, 20% of the population has social and private health insurance, while the remaining 30%, known as the "missing middle," have no health insurance.
- The Fifteenth Finance Commission recommends that the public health expenditure of the Union and States should be increased together to reach 2.5% of GDP (Growth Domestic Product) by 2025.
- According to the budget estimates for fiscal year 2020, about 1.35% of India's GDP was spent on public health. This was a slight increase compared to the previous fiscal year when about 1.29% of the GDP was spent on healthcare.
What are the Initiatives for the Health Care Sector?
- National Health Mission
- Ayushman Bharat.
- Pradhan Mantri Jan Arogya Yojana (AB-PMJAY).
- National Medical Commission
- PM National Dialysis Programme.
- Janani Shishu Suraksha Karyakram (JSSK).
- Rashtriya Bal Swasthya Karyakram (RBSK).
Conclusion
Inclusive healthcare is not just a matter of providing medical treatment; it is about creating a healthcare system that respects the dignity and rights of every individual. It requires addressing the diverse needs of all people, including those who are marginalized or vulnerable, and ensuring that healthcare services are accessible, affordable, and culturally competent. Inclusive healthcare is not only a moral imperative but also a practical necessity for achieving better health outcomes for all. By embracing inclusivity in healthcare, we can build healthier, more equitable societies where everyone has the opportunity to live a healthy and fulfilling life.
|
Drishti Mains Question: Discuss the challenges and strategies for achieving inclusive healthcare in India, highlighting the role of technology and policy reforms. What are the key areas for improvement? |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)