Governance
Optimizing India’s Healthcare System
- 08 Apr 2025
- 21 min read
This editorial is based on “Bridging gaps, building resilience” which was published in The Hindu on 07/04/2025. The article brings into picture the dual burden of diseases and healthcare disparities in India, highlighting how inadequate funding and high out-of-pocket expenses push millions into poverty. Despite schemes like Ayushman Bharat, access remains inequitable.
For Prelims: Ayushman Bharat, Ayushman Arogya Mandir, Artificial intelligence Application in Healthcare, Ayushman Bharat Digital Mission, National Tele Mental Health Programme , One Health approach, Non-communicable diseases, Zoonotic diseases, Antimicrobial resistance
For Mains: Key Recent Developments in India’s Healthcare Infrastructure and Resilience, Key Issues Associated with India’s Healthcare System.
India's healthcare system faces a dual burden of persistent infectious diseases and rising non-communicable conditions, with challenges including rural-urban infrastructure disparities and insufficient public health funding. Despite progress through initiatives like Ayushman Bharat and digital health platforms, inequitable access remains a concern. High out-of-pocket spending pushes 55 million Indians into poverty annually, highlighting the urgent need for increased investment in preventive care and universal coverage.
What are the Key Recent Developments in India’s Healthcare Infrastructure and Resilience?
- Infrastructure:
- Expansion of Health and Wellness Centers: The Indian government is expanding primary healthcare services through the establishment of Ayushman Arogya Mandir.
- This expansion addresses critical gaps in rural healthcare infrastructure by offering services like early disease detection, maternal and child health, and non-communicable disease management.
- As of February 2025, over 1.7 lakh Ayushman Arogya Mandir have been operationalized across India, aiming to cater to the population in underserved rural areas.
- Investment in Advanced Medical Technology and AI Integration: India's healthcare infrastructure has increasingly integrated cutting-edge medical technologies and artificial intelligence (AI) to improve diagnostics, treatment outcomes, and patient care.
- This includes AI-powered medical devices, robotic surgery tools, and predictive analytics in hospitals to better manage patient flows and resource allocation.
- For instance, Apollo Hospitals bets on AI to tackle staff workload, while DNA Wellness has announced an investment of Rs. 200 crore to set up 100 cervical cancer screening labs across India.
- Expansion of Medical Colleges: To tackle the growing healthcare demands in India, the government has accelerated the establishment of new AIIMS and medical colleges.
- The move aims to address the shortage of healthcare professionals, particularly in rural areas, and improve the availability of specialized medical care.
- For instance, according to a 2021 report by the government, 22 AIIMS are in different phases of development across the country,
- Expansion of Health and Wellness Centers: The Indian government is expanding primary healthcare services through the establishment of Ayushman Arogya Mandir.
- Resilience:
- Telemedicine and Digital Health Solutions: India has significantly improved its healthcare resilience through the adoption of digital health solutions, especially telemedicine.
- The Ayushman Bharat Digital Mission (ABDM) has created 73 crore Health Accounts (ABHA), enabling a seamless, digital exchange of health records across institutions
- As of 6th April, 2025, e-Sanjeevani has served over 36 crore patients through teleconsultations since its launch in 2020.
- The telemedicine market in India is expected to reach US$ 5.4 billion by FY25, reflecting the growing importance of digital solutions in healthcare resilience.
- Pharmaceutical Industry Growth: India's pharmaceutical sector has emerged as a major pillar of healthcare resilience, playing a crucial role in the global supply of vaccines and essential medicines.
- The country's ability to produce and distribute COVID-19 vaccines at an unprecedented scale, alongside its leadership in vaccine exports, has significantly boosted its health resilience.
- For instance, India has administered over 220 crore COVID-19 vaccine doses, with 30 crore doses exported.
- Investment in Mental Health Services and Tele Mental Health: In recognition of the growing mental health crisis, India has prioritized tele-mental health services, particularly through the National Tele Mental Health Programme (Tele MANAS), which offers remote access to psychological services.
- This initiative has expanded mental health resilience by ensuring that citizens across the country, especially in remote areas, have access to mental health care.
- As on 1st April 2025, 36 States/ UTs have already set up 53 Tele MANAS Cells to provide mental health support nationwide.
- Telemedicine and Digital Health Solutions: India has significantly improved its healthcare resilience through the adoption of digital health solutions, especially telemedicine.
What are the Key Issues Associated with India’s Healthcare System?
- Inequitable Access to Healthcare Service: India grapples with significant disparity in healthcare access between urban and rural areas.
- Despite numerous government initiatives, rural India continues to face severe shortages in both healthcare infrastructure and medical professionals, leading to unequal health outcomes.
- The concentration of healthcare resources in urban areas exacerbates these disparities.
- Approximately 70% of India’s population lives in rural areas, but only 35-40% of healthcare infrastructure is located there.
- Moreover, rural areas have only 1.7 nurses per 1,000 people, far below the global standard of 3-4 per 1,000.
- High Out-of-Pocket Expenditure: India’s healthcare system still remains heavily dependent on out-of-pocket expenditure, which pushes millions of Indians into poverty every year.
- While government schemes like Ayushman Bharat aim to reduce the financial burden on families, the overall reliance on private healthcare facilities continues to escalate.
- As per National Health Accounts Estimates for India (2019-20), out-of-pocket spending on healthcare accounted for 47.1% of total health expenditure.
- It’s estimated that 55 million Indians fall below the poverty line every year due to healthcare costs.
- Fragmentation of Healthcare Delivery: India’s healthcare system remains fragmented, with a stark divide between public and private healthcare sectors.
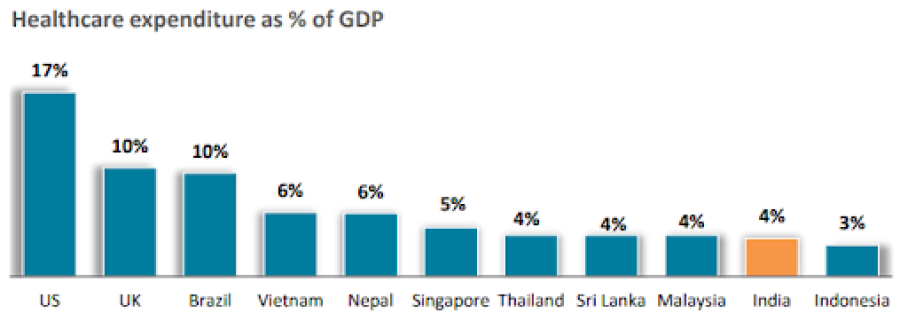
- The private sector provides a majority of secondary, tertiary, and quaternary care institutions with major concentration in metros, tier-I and tier-II cities, while public healthcare still struggles with a 1.9% of GDP expenditure.
- This fragmentation leads to inconsistent healthcare quality, where public health services are often underfunded and overwhelmed.
- Rising Burden of Non-Communicable Diseases (NCDs): India is facing a dual burden of diseases, with an increasing prevalence of non-communicable diseases (NCDs) like diabetes, hypertension, and cardiovascular diseases, alongside traditional infectious diseases.
- The rising prevalence of NCDs is attributed to sedentary lifestyles, poor diet, and tobacco use (as cited in Economic Survey 2023-24 as well), further straining an already burdened healthcare system.
- An estimated 5-6 million Indians lose their lives annually due to NCDs. 22% of Indians aged 30+ are at risk of dying from an NCD before the age 70.
- Inefficiencies in Healthcare Management and Governance: India’s healthcare management system is often criticized for inefficiencies and lack of coordination between central and state governments.
- Despite policy frameworks like the National Health Policy 2017, implementation challenges persist, particularly in terms of governance, data collection, and quality assurance.
- These issues impede the overall effectiveness of health programs, resulting in fragmented services and delayed responses to emerging health crises.
- For instance, the PM-JAY scheme has covered over 55 Crore individuals, but issues in fraud detection and service delivery quality continue to undermine its effectiveness.
- Recent, CAG report on the Ayushman Bharat scheme reveals irregularities, including invalid mobile numbers and potential fraud.
- Challenges in Universal Health Coverage: Despite significant strides in improving healthcare access, India still faces challenges in achieving Universal Health Coverage (UHC).
- Large swathes of the population, particularly in rural and economically disadvantaged areas, remain outside the formal health insurance system.
- While Ayushman Bharat has made considerable progress, systemic barriers and lack of awareness about available schemes continue to hinder UHC.
- Over 73 crore Ayushman Bharat Health Accounts have been created, but the coverage of health insurance remains limited, with only 33.33% share of the total health premiums underwritten by health insurance in FY24.
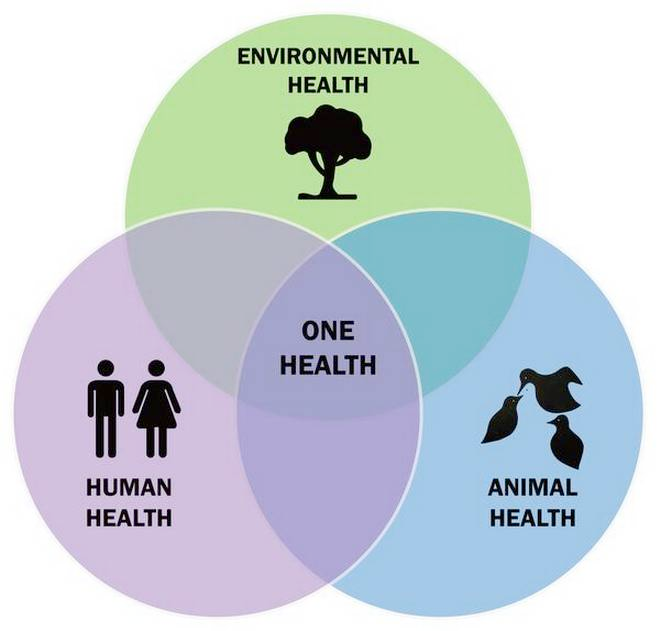
- Neglect of Environmental Health and One Health Approach: Environmental factors like air and water pollution are increasingly recognized as major health risks, yet efforts to mitigate these risks remain inadequate.
- Poor air quality in major cities contributes to respiratory diseases and cardiovascular conditions, severely impacting public health.
- The lack of effective environmental health policies exacerbates this issue, especially in urban centers with high pollution levels.
- Air pollution was responsible for 1.6 million deaths in India in 2019. In major cities like Delhi, air quality often worsens to hazardous levels.
- Also, given India's vulnerability to zoonotic diseases like Nipah, avian influenza, and increasing antimicrobial resistance (AMR), the absence of an integrated framework is a critical gap.
- Poor air quality in major cities contributes to respiratory diseases and cardiovascular conditions, severely impacting public health.
What Lessons India Can Learn from Other Countries in Terms of Healthcare?
- Thailand: Universal Health Coverage (UHC)
- Thailand’s UHC provides near-universal health access through an efficient public insurance model, minimizing financial barriers.
- India can adopt a similar system to offer universal health coverage that ensures affordable care for all, especially in rural areas
- Thailand’s UHC provides near-universal health access through an efficient public insurance model, minimizing financial barriers.
- Cuba: Primary Healthcare Focus
- Cuba emphasizes preventive care and strong primary healthcare systems, with doctors placed in communities for early detection.
- India could replicate this by enhancing Primary Health Centers (PHCs) and preventive services to tackle health issues before they escalate.
- Cuba emphasizes preventive care and strong primary healthcare systems, with doctors placed in communities for early detection.
- Germany: Health Insurance Expansion
- Germany’s dual public-private insurance system provides universal coverage, balancing public access with private choice.
- India can adopt a hybrid system to ensure broader coverage while maintaining quality care
- Germany’s dual public-private insurance system provides universal coverage, balancing public access with private choice.
- Estonia: Digital Health Integration
- Estonia’s digital health system provides universal electronic health records for seamless healthcare delivery.
- India can scale its digital health platforms to integrate electronic health records across all services.
- Estonia’s digital health system provides universal electronic health records for seamless healthcare delivery.
- Sweden: Healthcare Financing
- Sweden uses progressive taxation to fund healthcare, ensuring it’s free at the point of service.
- India can think of similar progressive tax system to reduce out-of-pocket spending and increase public healthcare funding (though healthcare cess is already there)
- Sweden uses progressive taxation to fund healthcare, ensuring it’s free at the point of service.
- Ethiopia: Community Health Workers
- Ethiopia uses community health workers to deliver care in remote areas, improving access.
- India can expand and secure the role of community health workers like ASHA by providing them a social safety net.
- Ethiopia uses community health workers to deliver care in remote areas, improving access.
What Measures India Can Adopt to Enhance its Healthcare System
- Strengthening Rural Healthcare Infrastructure with Telemedicine Integration: To bridge the urban-rural healthcare divide, India must significantly enhance rural healthcare infrastructure by expanding Ayushman Arogya Mandir and integrating them with telemedicine platforms.
- Telemedicine should be further leveraged to provide specialist consultations in remote areas, reducing the reliance on urban centers.
- This combination can improve accessibility, reduce the burden on tertiary hospitals, and ensure primary care in underserved regions.
- Public-Private Partnerships (PPPs) for Expanding Healthcare Coverage: India should expand the use of Public-Private Partnerships (PPPs) to enhance both infrastructure and healthcare delivery.
- The government can collaborate with private healthcare providers to set up more medical facilities in underserved regions and offer affordable care through insurance schemes like Ayushman Bharat.
- By aligning the goals of public and private stakeholders, India can increase capacity, streamline services, and enhance accessibility while maintaining quality standards across the system.
- Revamping Primary Healthcare with a Focus on Preventive Care: India should prioritize preventive healthcare at the Primary Healthcare Centers (PHCs) level to reduce the burden of non-communicable diseases (NCDs).
- This can be done through enhanced screening programs, health education, and early detection of diseases like diabetes and hypertension.
- By implementing early interventions and ensuring consistent follow-ups, the pressure on secondary and tertiary healthcare facilities can be reduced, improving the overall efficiency and cost-effectiveness of the system.
- Integrating Mental Health into the Primary Healthcare System: Mental health services must be integrated into the mainstream healthcare system by offering training to primary healthcare providers.
- This integration would ensure that mental health support is easily accessible across all regions, especially in underserved areas.
- By mainstreaming mental health care through public health programs and including it as part of routine medical check-ups, India can address the rising mental health burden more effectively and reduce stigma.
- Streamlining Health Insurance Schemes for Universal Coverage: To move towards Universal Health Coverage (UHC), India must streamline its health insurance schemes by expanding coverage to include outpatient care.
- Simplifying the claims process and ensuring quicker reimbursement timelines would make these schemes more accessible to vulnerable populations.
- Coordination between national and state health insurance schemes, along with improved awareness and outreach, would help ensure that the majority of the population benefits from comprehensive coverage.
- Fostering Digital Health Innovations and Data Integration: India should accelerate the integration of digital health solutions, such as electronic health records (EHRs), Ayushman Bharat Digital Mission (ABDM), and telemedicine platforms, to create a seamless and interoperable health data ecosystem.
- This would enable better management of health data, improve service delivery, and ensure that patients receive coordinated care across different healthcare providers.
- Implementing AI-based diagnostic tools and remote patient monitoring systems will further enhance healthcare quality, particularly in resource-poor settings.
- Implementing a National Health Workforce Strategy: India needs to implement a national health workforce strategy that includes comprehensive workforce planning, skill development programs, and retention strategies.
- This should be linked with incentives for professionals to work in underserved areas and incentives for further education.
- Streamlining the regulatory frameworks for training and certification of healthcare workers can ensure that the workforce is adequately equipped to meet the country’s diverse healthcare needs.
- Increasing Health Financing and Allocating More to Public Health: India should increase public healthcare spending to 2.5% of GDP as recommended by the 15th Finance Commission and ensure that the funds are allocated effectively.
- This can include enhanced financing for primary healthcare, investment in preventive healthcare programs, and upgrading the national healthcare infrastructure.
- Addressing Environmental Health and Strengthening the One Health approach: Environmental health, particularly air pollution, should be prioritized as a key public health issue. India can adopt stringent pollution control policies, incentivize green technologies, and invest in air quality monitoring systems.
- Linking these efforts with healthcare programs focusing on respiratory diseases will help mitigate the health effects of air pollution.
- Strengthening the One Health approach is essential for early disease detection, preventing outbreaks, and ensuring a holistic public health response in a world marked by climate change and global mobility.
Conclusion
India’s healthcare system is evolving, but persistent gaps in access, affordability, and infrastructure remain. Strengthening primary care, leveraging digital health, and reducing out-of-pocket expenditure are vital for building a resilient, inclusive system. Aligning with SDG 3 (Good Health and Well-being), India must prioritize universal health coverage through targeted investment, robust governance, and equitable service delivery.
|
Drishti Mains Question: Critically analyze the current state of healthcare infrastructure in India. What measures can be taken to ensure equitable access to quality healthcare across rural and urban areas? |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)