Governance
Bridging Gaps in India’s Health System
- 13 Nov 2024
- 18 min read
This editorial is based on “SDG goals at risk in nations such as India due to declining health spending: Data” which was published in The Hindu on 13/11/2024. The article brings into focus the sharp decline in government health spending per capita in low and lower-middle-income countries, including India, threatening progress toward universal health coverage and SDG health targets amid persistent budget cuts projected through 2029.
For Prelims: Government health spending, Sustainable Development Goals, Extreme weather events, Vector-borne diseases, antimicrobial resistance, Central Drug Regulator, National Mental Health Survey, zoonotic diseases, H3N2 influenza, Clinical Establishments Act of 2010, Ayushman Bharat Digital Mission, Active Pharmaceutical Ingredient.
For Mains: Key Emerging Health Challenges that India is Facing, Issues Related to Healthcare in India.
According to a recent paper published by the World Bank, low and middle-income countries, including India, are facing a decline in public health expenditure, reversing pre-pandemic gains. A study of 63 nations shows a drop in health spending growth from 2.4% (pre-pandemic) to 0.9% (2019-2023). In India and 34 other countries, health budgets have also fallen as a share of national spending, down to 6.5% in 2023. IMF projections indicate continued budget cuts for healthcare through 2029, raising concerns about achieving universal health coverage and Sustainable Development Goals health goals amidst widening infrastructure gaps.
What are the Key Emerging Health Challenges that India is Facing?
- Climate Change-induced Health Crisis: Rising temperatures and extreme weather events in India are significantly impacting public health, with heat-related illnesses, respiratory diseases, and vector-borne diseases showing alarming increases.
- In India, 191 billion potential labor hours were lost due to heat exposure in 2022, an increase of 54% from 1991-2000.
- Also, waterborne diseases, which are exacerbated by the rising frequency of floods, pose a significant health risk in India.
- Floods often contaminate water sources, leading to outbreaks of diseases like cholera, dysentery, and typhoid.
- Deaths due to extreme weather events rose 18% in India in just 3 years, with notable increases in vector-borne diseases like dengue.
- In India, 191 billion potential labor hours were lost due to heat exposure in 2022, an increase of 54% from 1991-2000.
- Antimicrobial Resistance (AMR) Crisis: India faces a critical challenge with antimicrobial resistance, driven by widespread misuse of antibiotics, poor sanitation, and inadequate healthcare practices.
- A 2022 Lancet study found that over 47% of antibiotic formulations used in India’s private sector in 2019 lacked approval from the Central Drug Regulator, leading to widespread and often unnecessary usage.
- Also, studies indicate a rise in multi-drug resistant infections in Indian hospitals, with reports of resistant strains of E. coli and Klebsiella pneumoniae increasingly found in intensive care units (ICUs).
- Mental Health Emergency: Post-pandemic India is witnessing an unprecedented mental health crisis, with inadequate infrastructure and workforce to address growing needs.
- The stigma surrounding mental health, combined with limited access to quality care and insufficient insurance coverage, creates significant barriers to treatment.
- Covid-19 pandemic triggered 25% increase in prevalence of anxiety and depression worldwide (WHO)
- The National Mental Health Survey indicates that 150 million Indians need mental health interventions, while there are only 0.75 psychiatrists per 100,000 population.
- Rising Non-communicable Diseases (NCDs): India's epidemiological transition shows a dramatic shift toward NCDs, particularly diabetes, cardiovascular diseases, and cancers, affecting younger populations and creating a double burden of disease.
- The combination of sedentary lifestyles, urbanization, and dietary changes is accelerating this trend, while healthcare systems struggle to adapt from infectious disease management to chronic care models.
- NCDs are a major global health issue, causing 74% of deaths worldwide and 63% of deaths in India.
- India now has more than 101 million people living with diabetes compared to 70 million people in 2019
- Double Burden of Diseases: India faces a "double burden of disease," dealing with both communicable and non-communicable diseases (NCDs) simultaneously.
- Infectious diseases like tuberculosis, dengue, and malaria remain widespread, especially in rural and low-income areas.
- Post-Covid-19 pandemic, India faces new challenges from emerging and re-emerging infectious diseases, with increasing concerns about zoonotic diseases and pandemic preparedness.
- India reported over 3,000 cases of H3N2 influenza in 2023.
- In India, 30 Mpox cases have been reported since the WHO's 2022 PHEIC Declaration.
- Post-Covid-19 pandemic, India faces new challenges from emerging and re-emerging infectious diseases, with increasing concerns about zoonotic diseases and pandemic preparedness.
- Meanwhile, the rise of NCDs such as diabetes, hypertension, cancer and cardiovascular diseases is accelerating due to lifestyle changes, urbanization, and dietary shifts.
- Studies have estimated a 12.8% increase in the number of annual cancer cases by the year 2025, which would be around 1.57 million.
- This dual challenge strains healthcare resources, as facilities must address both communicable diseases and chronic conditions that require long-term care.
- Infectious diseases like tuberculosis, dengue, and malaria remain widespread, especially in rural and low-income areas.
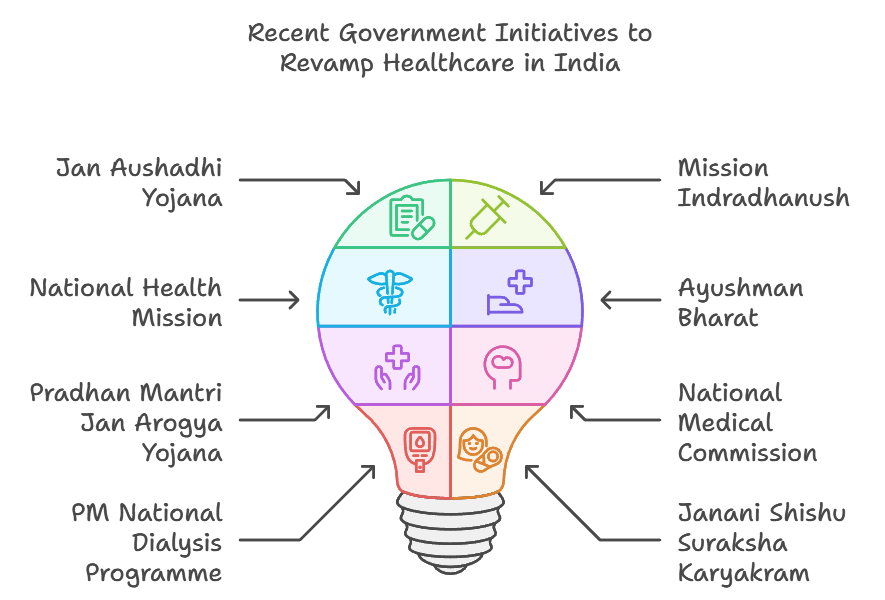
Why is India Struggling to Sustain Effective Healthcare Despite Multiple Initiatives?
- Fragmented Governance: India's healthcare system suffers from fragmented governance across central, state, and local levels, leading to inconsistent policy implementation and resource allocation.
- States like Kerala have robust healthcare systems with better health indicators, while others like Bihar lag behind.
- The Clinical Establishments Act of 2010 aims to standardize healthcare services across India.
- However, its implementation varies by state, leading to differences in healthcare quality and regulation enforcement.
- Inadequate Health Care Financing: Despite ambitious healthcare initiatives, India's public health spending remains critically low, with heavy reliance on private out-of-pocket expenditure.
- Government health expenditure in India stands at 1.9% of GDP, as per the Economic Survey 2023-24.
- In India, out-of-pocket health expenditure (OOP) expenses account for about 62.6% of total health expenditure, one of the highest in the world
- Infrastructure and Resource Disparities: Urban-rural divide in healthcare infrastructure continues to widen, with significant disparities in the distribution of medical facilities, equipment, and infrastructure.
- Only 11% of sub-centers, 13% of PHCs, and 16% of CHCs meet Indian Public Health Standards.
- A Niti Aayog report has said that about 65% of hospital beds in the country cater to almost 50% of the population.
- Workforce Challenges and Brain Drain: The healthcare sector faces severe shortages of qualified professionals, compounded by continuous brain drain and uneven distribution.
- Medical education capacity, though expanding, struggles with quality issues and doesn't align with healthcare needs. Rural postings remain unattractive despite incentives.
- The Rural Health Statistics report shows that there is a shortfall of more than 80% of the required surgeons and pediatricians in the 6,064 Community Health Centres across the country.
- Data Management and Monitoring Gaps: Despite digital initiatives, healthcare data remains poorly integrated, hampering evidence-based policy-making and resource allocation.
- The lack of real-time health surveillance systems affects disease monitoring and response capabilities.
- Privacy concerns and infrastructure limitations slow digital health adoption.
- Despite the government’s efforts to promote Ayushman Bharat Digital Mission adoption, only 30% of total Health Facility Registry have come from the private sector, despite holding a 70% market share.
- Lack of Focus on Preventive healthcare: Focus remains predominantly on curative care rather than preventive healthcare and public health measures.
- Health education and awareness programs receive inadequate attention and resources. Environmental health and social determinants of health get limited policy focus.
- The Indian government's expenditure on preventive healthcare constitutes only 13.55% of the Current Health Expenditure (CHE).
- Supply chain and pharmaceutical issues: Healthcare supply chains remain inefficient with frequent stockouts of essential medicines and equipment.
- Dependence on imported active pharmaceutical ingredients affects drug security and costs.
- Generic medicine programs face implementation and quality perception challenges.
- India imports about 70% of its Active Pharmaceutical Ingredient requirements from China, particularly vitamins and antibiotics.
- Dependence on imported active pharmaceutical ingredients affects drug security and costs.
What Measures can India Adopt to Strengthen the Healthcare System?
- Integrated Digital Health Ecosystem: India should fast-track the implementation of the Ayushman Bharat Digital Mission by establishing a unified health data infrastructure that connects all stakeholders, from primary health centers to tertiary hospitals.
- This would include standardized Electronic Health Records (EHRs), telemedicine platforms, and real-time disease surveillance systems, while ensuring robust data privacy and security.
- The system must allow seamless information exchange between public and private healthcare providers, with a focus on improving last-mile connectivity in rural areas.
- Also, platforms like E-Sanjeevani can be expanded and strengthened learning from Tamil Nadu which has topped eSanjeevani OPD consultations as per a 2020 report.
- Strengthening Primary Health Care: Health and Wellness Centers (HWCs) should be transformed into comprehensive primary care hubs, equipped with essential diagnostics, telemedicine facilities, and trained personnel.
- The focus should shift to preventive care and early detection through regular health screenings, vaccination programs, and community health education.
- A strong referral system should connect primary, secondary, and tertiary care facilities, while local communities, through ASHAs and community health workers, can be engaged for better health awareness and preventive care.
- Performance-based incentives for healthcare workers would also improve service quality and retention.
- Public-Private Partnership Reforms: New Public-Private Partnership (PPP) models should be developed to ensure equitable healthcare access while maintaining high-quality standards.
- Clear regulatory frameworks with performance metrics, quality benchmarks, and pricing controls should be implemented for private sector participation.
- Independent monitoring systems should be established to assess PPP outcomes and ensure accountability.
- Furthermore, technology transfer and capacity building should be a focus of these partnerships.
- Healthcare Financing Reform: A mixed financing model should be adopted, combining increased public spending with universal health insurance coverage.
- Public health spending should gradually be increased to 2.5% of GDP through a dedicated health cess and optimized resource allocation.
- Strengthening the Ayushman Bharat scheme by expanding coverage and simplifying claim processes is essential.
- Recent expansion of health coverage under the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana to include all senior citizens aged 70 and above is a significant step.
- Medical Education and Workforce Development: Medical education should be modernized with a focus on practical skills, digital health, and emerging technologies.
- A mandatory rural posting system with attractive incentives and career progression opportunities should be introduced.
- Chhattisgarh’s Mitanin program, which uses community health workers effectively to address rural doctor shortages, can serve as a model.
- A standardized continuing medical education system with regular skill updates should be created. Additionally, medical education hubs should be established in underserved regions, with a focus on addressing local healthcare needs.
- A mandatory rural posting system with attractive incentives and career progression opportunities should be introduced.
- Pharmaceutical and Medical Device Manufacturing: India should strengthen domestic manufacturing capabilities for essential medicines and medical devices through Production Linked Incentive schemes.
- API parks with shared infrastructure should be developed to reduce import dependence.
- Quality control measures and standardization for generic medicines should be implemented to build trust in domestic products.
- The Jan Aushadhi network should also be strengthened with better supply chain management.
- Emergency Preparedness System: A network of regional emergency response centers should be established, with adequate surge capacity and essential supplies.
- Early warning systems for disease outbreaks, with real-time monitoring capabilities, should be implemented.
- Additionally, strategic reserves of essential medicines and equipment should be built and regularly rotated.
- Preventive Healthcare Focus: Comprehensive health screening programs should be implemented across all age groups at HWCs.
- Integrating traditional medicine systems (AYUSH) with modern medicine could offer a holistic approach to healthcare.
- Targeted interventions for lifestyle diseases should be introduced through workplace and school health programs.
- Campaigns like Eat Right India and Fit India should be actively promoted to encourage healthier lifestyles.
- Regulatory Framework Modernization: A unified healthcare regulatory authority should be established with clear mandates for quality control and standard setting.
- Mandatory accreditation systems for all healthcare facilities should be implemented, with regular audits.
- Transparent pricing mechanisms for medical services and procedures should be developed.
- One Health Approach: India should fast track the implementation of the One Health approach, which links human, animal, and environmental health to prevent zoonotic diseases.
- Strengthening surveillance and early detection systems at the human-animal-environment interface can help control outbreaks.
- Collaboration between healthcare, veterinary, and environmental sectors is essential.
Conclusion:
To address India's mounting healthcare challenges, a multi-pronged approach is essential, focusing on digital integration, preventive care, and robust public-private partnerships.Strengthening primary care and emphasising preventive health will reduce the burden on tertiary systems. With coordinated reforms, India can better navigate health crises and advance towards universal health coverage and Sustainable Development Goals (SDGs).
|
Drishti Mains Question: Analyse the key challenges faced by India's healthcare system and suggest measures to strengthen its effectiveness and accessibility for all sections of society. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)