UK’s Assisted Dying Bill on Terminally ill Adults | 05 Dec 2024
Why in News?
Recently, the UK House of Commons voted in favour of the Terminally Ill Adults (End of Life) Bill, allowing terminally ill patients to request assistance to end their own lives.
- This landmark decision reflects ongoing debates about end-of-life rights and raises questions about ethical considerations and legal frameworks.
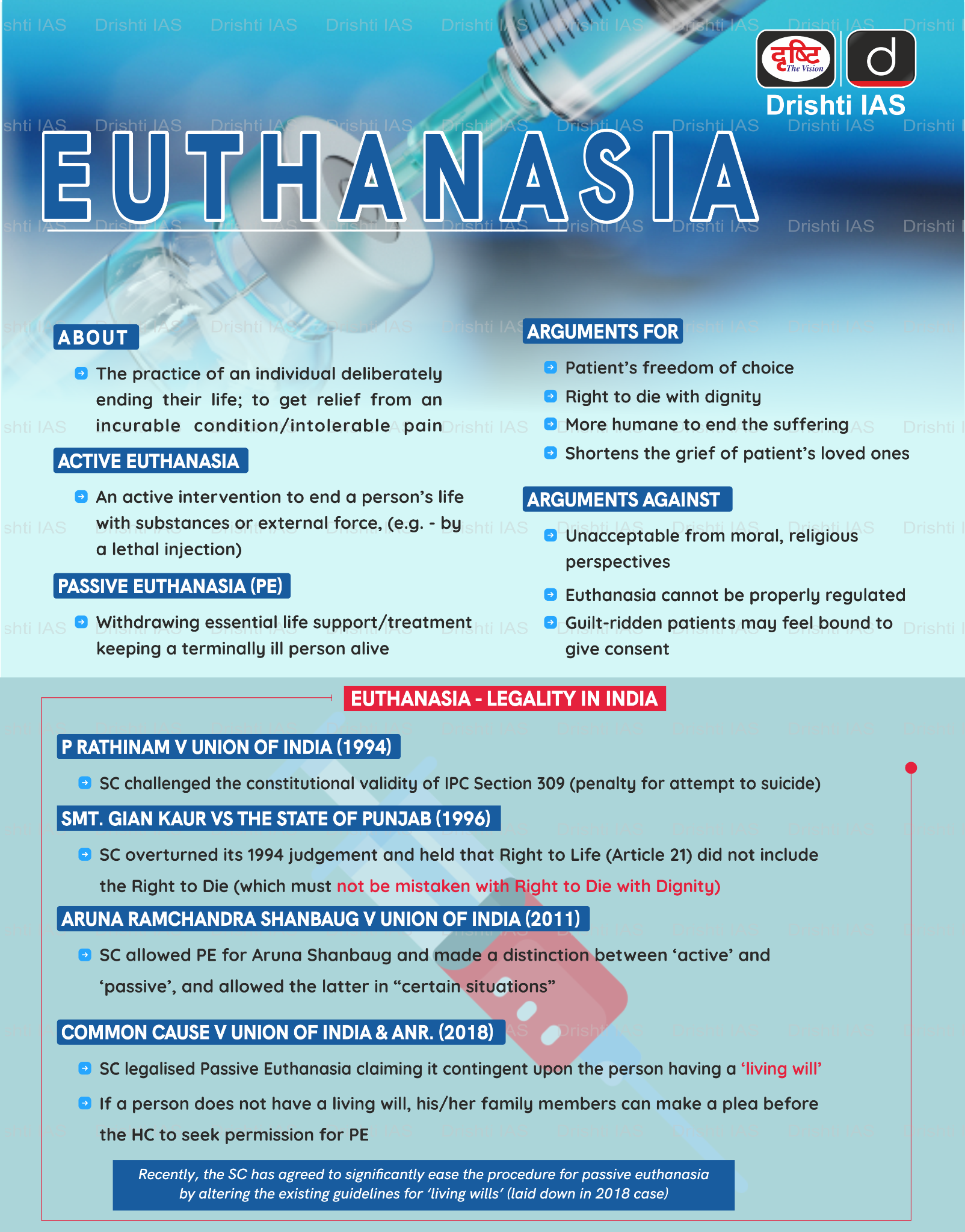
Assisted dying refers to both voluntary active euthanasia and physician-assisted death.
Euthanasia involves a doctor actively ending the life of a terminally ill patient.
What are the Key Highlights of the UK’s Assisted Dying Bill?
- Current Position of UK on Assisted Dying:
- The Suicide Act 1961 makes it illegal to encourage or assist a suicide in England, Wales and Northern Ireland.
- Assisted suicide is considered an offence and can be punished with up to 14 years in prison.
- Since 2013, at least three bills have been introduced to allow assisted dying in the UK.
- The Suicide Act 1961 makes it illegal to encourage or assist a suicide in England, Wales and Northern Ireland.
- Terminally Ill Adults (End of Life) Bill:
- Definition of Terminal Illness: A terminally ill person is defined as someone with a worsening condition that cannot be reversed by treatment and is expected to die within 6 months.
- The bill explicitly excludes individuals with disabilities or mental disorders.
- Eligibility Criteria: Only terminally ill individuals aged 18 and above with mental capacity can request assisted dying.
- Patients must be registered and residing in England or Wales for at least 12 months prior to the request.
- In the United Kingdom, each nation and crown dependency is responsible for its own health care, so Scotland and Northern Ireland would have to pass their own assisted-dying rules.
- Patients must be registered and residing in England or Wales for at least 12 months prior to the request.
- Request Process:
- Patients must sign a "first declaration" in the presence of a coordinating doctor and a witness.
- First Declaration: A person who wishes to be provided with assistance to end their own life in accordance with this Act must make a declaration to that effect.
- The coordinating doctor conducts an initial assessment to confirm eligibility and voluntary consent.
- If approved, the request is referred to an independent doctor after a minimum seven-day reflection period.
- Patients must sign a "first declaration" in the presence of a coordinating doctor and a witness.
- Judicial Oversight:
- If both doctors (coordinating and independent) agree, the request is sent to the High Court of Justice, which verifies compliance with legal requirements.
- The court can question both the patient and the doctors involved.
- If both doctors (coordinating and independent) agree, the request is sent to the High Court of Justice, which verifies compliance with legal requirements.
- Final Confirmation:
- A second reflection period of 14 days follows judicial approval, after which the patient signs a second declaration witnessed by both doctors and another person.
- Self-Administration of Substance:
- The coordinating doctor provides an “approved substance” for self-administration by the patient, doctors are not authorized to administer it themselves.
- Definition of Terminal Illness: A terminally ill person is defined as someone with a worsening condition that cannot be reversed by treatment and is expected to die within 6 months.
Euthanasia Policies in Different Countries
- Netherlands, Luxembourg, Belgium: Allow both euthanasia and assisted suicide for those with "unbearable suffering" with no chance of improvement.
- Switzerland: Prohibits euthanasia but permits assisted dying with a doctor's presence.
- United States: Euthanasia laws vary by state, with allowances in states like Washington, Oregon, and Montana.
- France: Adults with French citizenship or residency, suffering from a severe illness and unbearable pain, can request lethal medication if they can express their wishes. Assistance is permitted if they cannot self-administer.
What are the Provisions of Living Will and Passive Euthanasia in India?
- Passive Euthanasia: Passive euthanasia involves withholding or withdrawing medical treatment to allow a person to die.
- In contrast, active euthanasia involves actively ending a person's life through substances or external force, like a lethal injection.
- BJudicial Stand: The Supreme Court of India, in its 2018 judgment in Common Cause vs. Union of India, recognized the "right to die with dignity" as part of Article 21 of the Constitution.
UPSC Civil Services Examination, Previous Year Question (PYQ)
Prelims
Q. Right to Privacy is protected as an intrinsic part of Right to Life and Personal Liberty. Which of the following in the Constitution of India correctly and appropriately imply the above statement? (2018)
(a) Article 14 and the provisions under the 42nd Amendment to the Constitution.
(b) Article 17 and the Directive Principles of State Policy in Part IV.
(c) Article 21 and the freedoms guaranteed in Part III.
(d) Article 24 and the provisions under the 44th Amendment to the Constitution.
Ans: (c)