Ethics
Passive Euthanasia
- 24 Aug 2024
- 7 min read
For Prelims: Passive euthanasia, National Health Digital Record, Article 21, Living Will.
For Mains: Major Changes in Guidelines of Passive Euthanasia, Euthanasia in India.
Why in News?
Recently, the Supreme Court of India denied a petition from an elderly couple seeking "passive euthanasia" for their comatose (deeply unconscious) son, who has been bedridden for 11 years following a fall.
- This ruling has reignited discussions on the legal and ethical dimensions of euthanasia in India.
What is the Background of the Case?
- The Supreme Court ruled against the patient’s parents' plea, stating that the case did not qualify as passive euthanasia since the patient was not on any life support systems and was receiving nutrition through a feeding tube.
- The court said that allowing him to die would not constitute passive euthanasia but rather active euthanasia, which remains illegal in India.
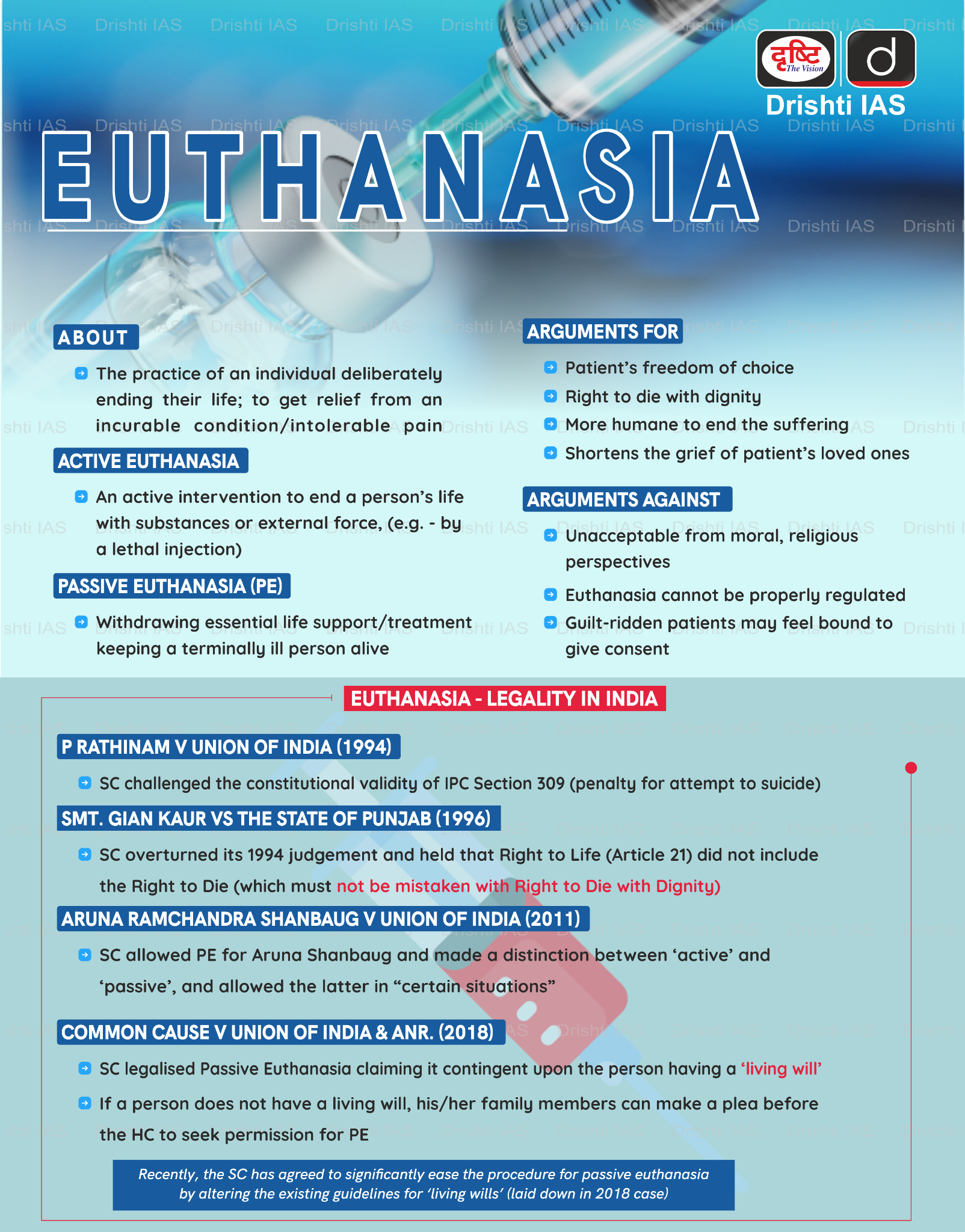
What is Passive Euthanasia?
- About:
- Euthanasia is the practice of ending the life of a patient to limit the patient's suffering.
- Types of Euthanasia:
- Active Euthanasia:
- Active euthanasia occurs when the medical professionals, or another person, deliberately do something that causes the patient to die, such as administering a lethal injection.
- Passive Euthanasia:
- Passive euthanasia is the act of withholding or withdrawing medical treatment, such as withholding or withdrawing life support, with the intention of allowing a person to die.
- Active Euthanasia:
- Euthanasia in India:
- The Supreme Court of India in a landmark judgement in Common Cause vs Union of India (2018) recognised a person’s right to die with dignity, saying that a terminally ill person can opt for passive euthanasia and execute a living will to refuse medical treatment.
- It also laid down guidelines for ‘living will’ made by terminally ill patients who beforehand know about their chances of slipping into a permanent vegetative state.
- Previously in 2011, the SC recognised passive euthanasia in the Aruna Shanbaug case for the first time.
- The court specifically stated that “Dignity in the process of dying is as much a part of the right to life under Article 21. To deprive an individual of dignity towards the end of life is to deprive the individual of a meaningful existence.”
- The Supreme Court of India in a landmark judgement in Common Cause vs Union of India (2018) recognised a person’s right to die with dignity, saying that a terminally ill person can opt for passive euthanasia and execute a living will to refuse medical treatment.
- Different Countries with Euthanasia:
- Netherland, Luxembourg, Belgium allows both types of euthanasia and assisted suicide for anyone who faces “unbearable suffering” that has no chance of improvement.
- Switzerland bans euthanasia but allows assisted dying in the presence of a doctor or physician.
- Since 1942, Switzerland has allowed assisted suicide, focusing on personal choice and control over the dying process. The law requires individuals to be of sound mind and their decision must not be driven by selfish motives.
- Australia has also legalised both types of euthanasia, and applies to adults with full decision-making capacity who have a terminal illness with a prognosis of death within six or twelve months.
- The Netherlands has a well-established legal framework for euthanasia, regulated by the “Termination of Life on Request and Assisted Suicide (Review Procedures) Act” of 2001.
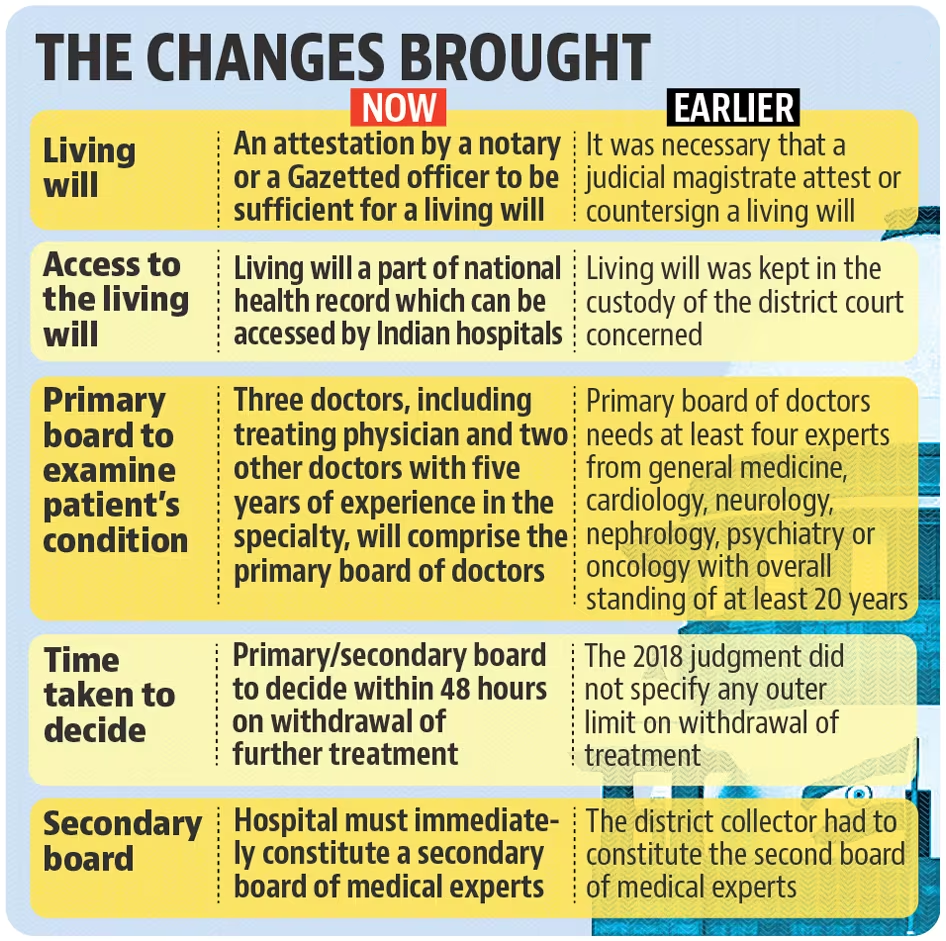
What were the Recent Changes in Guidelines made by the Supreme Court on Passive Euthanasia?
- The Supreme Court in 2023 modified the 2018 Euthanasia Guidelines to ease the process of granting passive euthanasia to terminally ill patients.
- In 2018 the Supreme Court recognised the Right to die with dignity as a fundamental right and prescribed guidelines for terminally ill patients to enforce the right.
- Modifications in SC Guidelines:
- Attestation of Living Will: The Court removed the requirement for a judicial magistrate's attestation on a living will. Now, attestation by a notary or a gazetted officer suffices, simplifying the procedure for individuals to express their end-of-life choices.
- Integration with National Health Digital Record: Previously, living wills were held by the district court. The revised guidelines mandate that these documents be part of the National Health Digital Record. This ensures easier access for hospitals and doctors nationwide, facilitating timely decision-making.
- Appeal Process for Denial of Euthanasia: If a hospital’s medical board denies permission to withdraw life support, the patient's family can appeal to the relevant High Court. The Court will then form a new medical board to reassess the case, ensuring a thorough and just review.
What are the Ethical Considerations of Euthanasia?
- Autonomy and Informed Consent: Euthanasia involves respecting individual autonomy, meaning people should have the right to decide about their own lives, especially to end suffering if they are mentally competent.
- It also requires informed consent, where the person must fully understand their condition, the euthanasia process, and its consequences to ensure they are not coerced or manipulated.
- Quality of Life vs. Sanctity of Life: Euthanasia debates often centre on quality of life, which argues that ending suffering and preserving dignity in severe illness can be ethical, versus sanctity of life, which holds that life is intrinsically valuable and should not be ended prematurely, often reflecting religious or philosophical beliefs.
- Legal and Social Implications: Euthanasia's legal framework varies by jurisdiction, reflecting different cultural attitudes and ethical debates on end-of-life issues.
- The social impact involves questions about medical professionals' roles, societal responsibilities, and the need for equitable access to palliative care and psychological support to address the underlying reasons for seeking euthanasia.
|
Drishti Mains Question: What is Active Euthanasia? What are the ethical and moral implications for this practice? |