Uttarakhand Switch to Hindi
Ayushman Yojana
Why in News
Recently, in Uttarakhand, the government has made changes in the system of treatment under the Ayushman scheme and has made it mandatory that now patients will be able to get treatment in empaneled private hospitals only after referring them from government hospitals.
Key Points
- It is noteworthy that the state government had given permission for direct private hospitalization during the Covid period, but now this exemption has been abolished as soon as the corona infection subsides.
- Referral has been made mandatory by the State Health Agency for Ayushman scheme for free treatment of five lakh rupees, but referral is not mandatory for treatment under the cashless state health scheme being run for government employees and pensioners i.e. patients directly enlisted can go to hospitals for treatment.
- However, the patients will get the facility of direct treatment in the NAVH accredited private hospitals of the state.
- It is known that Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PMJAY) is the world's largest health insurance scheme, which is fully funded by the Central Government.
- Under this, each beneficiary family is provided an insurance cover of Rs 5,00,000 per year for secondary and tertiary health treatment in public and private empaneled hospitals. Hospitalization and subsequent expenses (such as medical tests and medicines) are also covered under this plan.




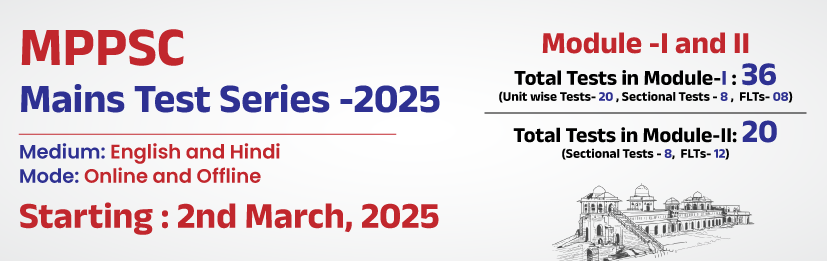
%20MPPCS%202025%20Desktop%20E.jpg)
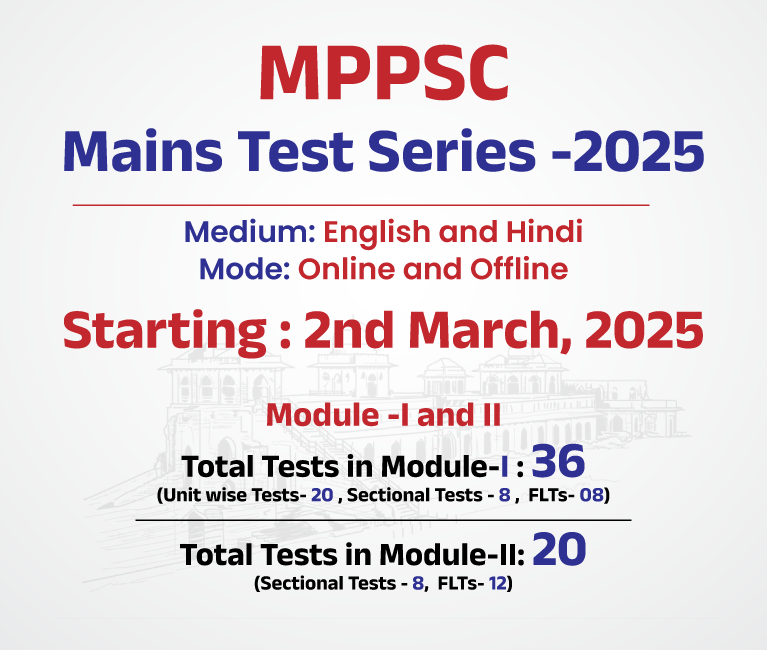
%20MPPCS%202025%20Mobile%20E%20(1).jpg)
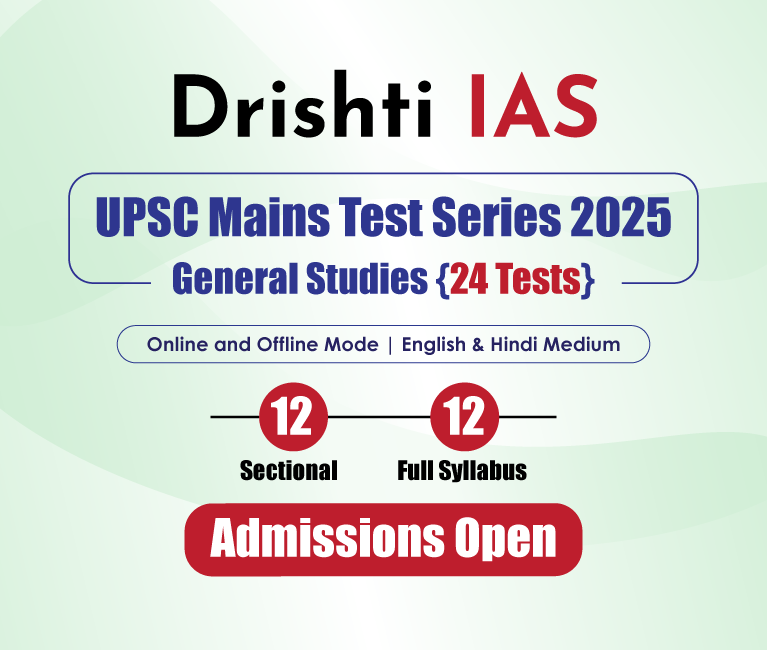
.png)
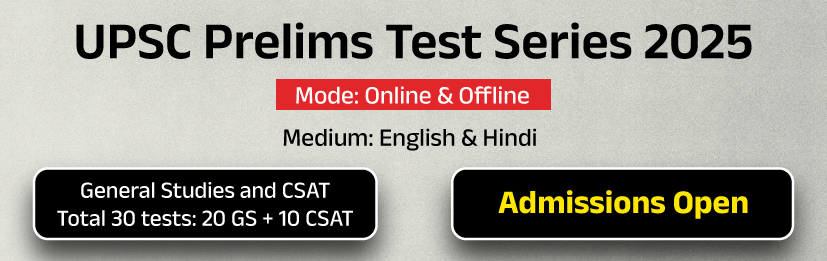
.png)



 PCS Parikshan
PCS Parikshan

