Indian Economy
A Digital Push For Healthcare
- 18 Aug 2020
- 9 min read
This editorial analysis is about the “A digital push for healthcare” which was published in The Indian Express on 14/08/2020. It talks about the need for digitisation of healthcare and challenges that lie ahead.
Recently, many digital initiatives have been launched in India such as the National Digital Health Blueprint, National Health Stack (NHS), etc. These initiatives are aimed at re-imagining India’s health data ecosystem.
The basic idea is that instead of ferrying medical records in polythene bags from doctor to doctor, Indian should be able to access their lab reports, x-rays and prescriptions irrespective of where they were generated, and share them with doctors or family members with consent.
Indeed these initiatives have intended benefits but there are many challenges in their implementation.
National Health Stack (NHS)
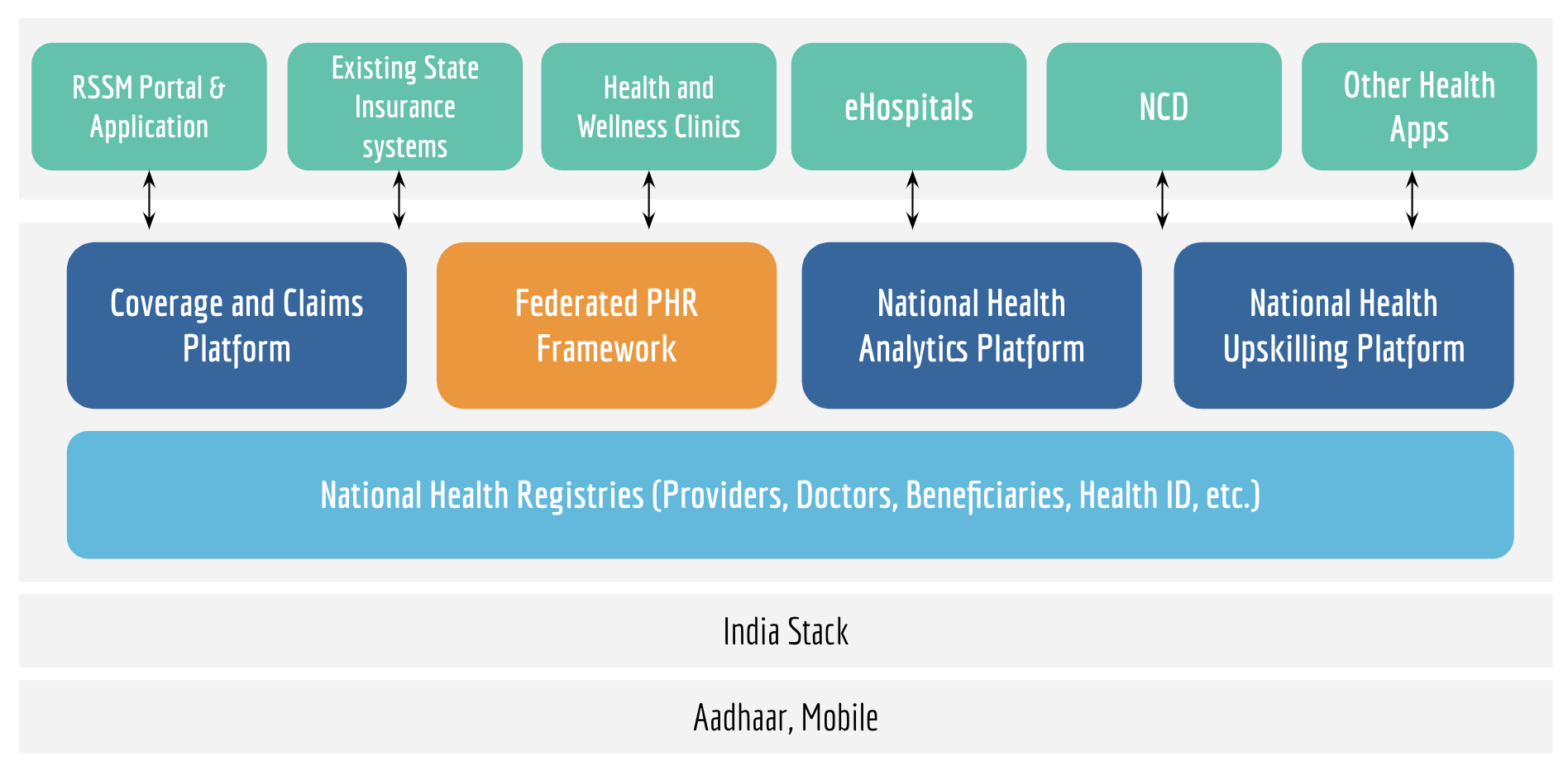
NHS is digital infrastructure built with the aim of making the health insurance system more transparent and robust, while factoring in the uniqueness of India’s health sector, and the political realities of federalism. There are five components of NHS:
- An electronic national health registry that would serve as a single source of health data for the nation;
- A coverage and claims platform that would serve as the building blocks for large health protection schemes, allow for the horizontal and vertical expansion of schemes like Ayushman Bharat by states, and enable a robust system of fraud detection;
- A federated personal health records (PHR) framework that would serve the twin purposes of access to their own health data by patients, and the availability of health data for medical research, which is critical for advancing the understanding of human health;
- A national health analytics platform that would provide a holistic view combining information on multiple health initiatives, and feed into smart policymaking, for instance, through improved predictive analytics; and
- Other horizontal components including a unique digital health ID, health data dictionaries and supply chain management for drugs, payment gateways, etc., shared across all health programmes.
National Digital Health Blueprint (NDHB)
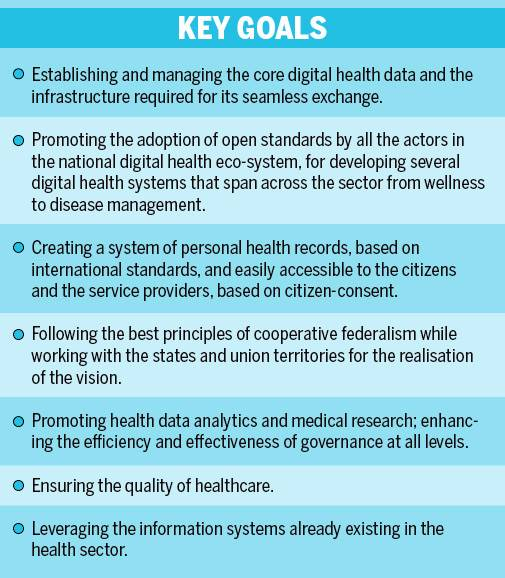
This National Digital Health Blueprint is an extension of the National Health Policy of 2017 (NHP 2017) that was formulated to provide universal healthcare to all citizens of India based on digital technologies for achieving higher efficiency and effectiveness.
- The NDHB is the architectural document for the implementation of the National Health Stack.
- The NDHB identifies the necessity to establish a specific organisation, called the National Digital Health Mission (NDHM) that can facilitate the implementation of the blueprint, to support and simplify the development of a national digital health ecosystem.
- The key features of this blueprint include a unified architecture, a set of architectural elements, a five-layered structure of architectural institutional blocks, a Unique Health ID (UHID), privacy and consent control, national portability, electronic health records, appropriate principles and guidelines, and health analytics.
- It also aims to deploy Artificial Intelligence (AI) in leveraging health records.
Intended Benefits
- Coherence Between Central and State Health Schemes: Currently, apart from Ayushman Bharat or Pradhan Mantri Jan Arogya Yojana (PMJAY), there are many secondary and tertiary care schemes running in the states.
- The initiatives like NDHB will help in creating synergy between union and states. Thereby, promoting the cause of cooperative federalism.
- Aiding Integration of Ayushman Bharat Scheme: Without integration between the two components (Health & wellness centres and PMJAY) of Ayushman Bharat Scheme, the goal of continuum of care cannot be met.
- NDHB and NHS will help in integration of the two arms of Ayushman Bharat.
- This will help in shifting focus from “Illness to Wellness” to drive down future cost of health protection.
- Interoperability of Health Schemes: NHS will also provide for a common digital language for the operationalisation and interoperability of various health schemes.
- Also the continuum of healthcare will be promoted as the NHS supports information flow across primary, secondary and tertiary healthcare.
- Effective Governance: Transparency principle that is imbibed in the NHS and NDHB will help in furtherance of effective public service delivery in many fronts. For example:
- Cashless Care to ensure financial protection to the poor.
- Timely Payments on Scientific Package Rates to service providers, a strong lever to participate in government-funded healthcare programs.
- Robust Fraud Detection to prevent funds leakage.
- Improved Policy Making through access to timely reporting on utilization and measurement of impact across health initiatives.
- Enhanced Trust and Accountability through non-repudiable transaction audit trails.
Associated Challenges
- Procedural Challenges: First, to enable seamless data exchange, all users must be incentivised or mandated to adopt a standard language of communication.
- A claims-driven documentation system, that also serves as a medico-legal instrument, runs the risk of reducing highly-trained professionals to data-entry operators who must enter billing and legal information, that has little relevance for clinical care.
- It is imperative that India, while embracing global standards, seriously rethinks what to document, when, why, and most importantly, by whom.
- Data Security and Privacy: One of the biggest concerns has been regarding data security and privacy of patients.
- The concerns were aggravated after an Assam minister and a senior official of the National Health Authority posted patient details on Twitter recently.
- The concerns with universal IDs are particularly salient when it comes to sensitive personal data like health data.
- More than a year after the Justice Srikrishna Committee prepared a draft data privacy law, there has been little meaningful movement on it.
Conclusion
- The National Health Stack will facilitate collection of comprehensive healthcare data across the country.
- Designed to leverage India Stack, subsequent data analysis on NHS will not only allow policy makers to experiment with policies, detect fraud in health insurance, measure outcomes and move towards smart policy making, it will also engage market players (NGOs, researchers, watchdog organizations) to innovate and build relevant services on top of the platform and fill the gaps.
- The portability of clinically-relevant data across private public divides and states will cut costs and save time, the ability to monitor compliance, say, with responsible use of antibiotics, can profoundly alter practice and improve the quality of care, and the ability to conduct timely institution-based syndromic surveillance may alter the course of an epidemic, and of a nation
- The design is geared to generate vast amounts of data resulting in some of the largest health databases with secured aggregated data that will put India at the forefront of medical research in the world.
|
Drishti Mains Question Explain how initiatives like National Health Stack will provide a much needed digital push in India’s health infrastructure. |
This editorial is based on “Limited peace: On UAE-Israel peace agreement” which was published in The Hindu on August 15th, 2020. Now watch this on our Youtube Channel.