Science & Technology
Mucormycosis Fungal Infection
- 15 Dec 2020
- 6 min read
Why in News
Recently, doctors have witnessed increased cases of Covid-19 triggered Mucormycosis.
- The reduced immunity of Covid-19 patients makes them more susceptible to this fungal infection.
Key Points
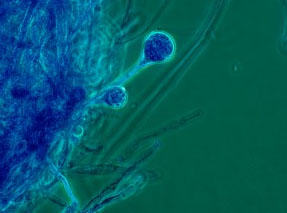
- Mucormycosis is also called Black Fungus or Zygomycosis and is a serious but rare fungal infection caused by a group of molds called mucormycetes.
- Types of Mucormycosis:
- Rhinocerebral (Sinus and Brain) Mucormycosis: It is an infection in the sinuses that can spread to the brain. It is the most common in people with uncontrolled diabetes and in people who have had a kidney transplant.
- Pulmonary (Lung) Mucormycosis: It is the most common type of mucormycosis in people with cancer and in people who have had an organ transplant or a stem cell transplant.
- Gastrointestinal Mucormycosis: It is more common among young children than adults, especially premature and low birth weight infants less than 1 month of age, who have had antibiotics, surgery, or medications that lower the body’s ability to fight germs and sickness.
- Cutaneous (Skin) Mucormycosis: It occurs after the fungi enter the body through a break in the skin (for example, after surgery, a burn, or other types of skin trauma). It is most common among people who do not have weakened immune systems.
- Disseminated Mucormycosis: It occurs when the infection spreads through the bloodstream to affect another part of the body. The infection most commonly affects the brain, but also can affect other organs such as the spleen, heart, and skin.
- Transmission:
- It occurs through inhalation, inoculation, or ingestion of spores from the environment.
- For example, the lung or sinus forms of the infection can occur after someone inhales the spores from the air.
- Mucormycosis does not spread between people or between people and animals.
- It usually occurs in people who have health problems or take medicines that lower the body’s ability to fight germs and sickness.
- It occurs through inhalation, inoculation, or ingestion of spores from the environment.
- Symptoms:
- General symptoms are one-sided facial swelling and numbness, headache, nasal or sinus congestion, black lesions on nasal bridge or upper inside of the mouth, fever, abdominal pain, nausea and gastrointestinal bleeding.
- Disseminated mucormycosis typically occurs in people who are already sick from other medical conditions, so it can be difficult to know which symptoms are related to mucormycosis. Patients with disseminated infection in the brain can develop mental status changes or coma.
- Diagnosis and Testing:
- Healthcare providers consider medical history, symptoms, physical examinations, and laboratory tests when diagnosing mucormycosis.
- If suspected of the infection, healthcare providers collect a sample of fluid from the respiratory system or may perform a tissue biopsy.
- In tissue biopsy, a small sample of affected tissue is analysed in a laboratory for evidence of mucormycosis under a microscope or in a fungal culture.
- Treatment:
- It needs to be treated with prescription antifungal medicine to prevent mucormycosis and other mold infections.
- Often, mucormycosis requires surgery to cut away the infected tissue.
- Prevention and Cure:
- There is no vaccine to prevent mucormycosis and it is difficult to avoid breathing in fungal spores because the fungi are common in the environment.
- For people who have weakened immune systems, there may be some ways to lower the chances of developing mucormycosis.
- These include avoiding areas with a lot of dust like construction or excavation sites, avoiding direct contact with water-damaged buildings and flood water after hurricanes and natural disasters and avoiding activities that involve close contact to soil.
- Early detection can prevent loss of eyesight, nose or jaw through clinical intervention.
- Mucormycetes, the group of fungi that cause mucormycosis, are present throughout the environment, particularly in soil and in association with decaying organic matter, such as leaves, compost piles, and animal dung.
- Several different types of fungi can cause mucormycosis and belong to the scientific order Mucorales.
- The most common types that cause mucormycosis are Rhizopus species and Mucor species.
- They are more common in soil than in air, and in summer and fall than in winter or spring.
- These fungi are not harmful to most people but for people who have weakened immune systems, breathing in micromycetes spores can cause an infection.