Governance
Best Practices in the Performance of District Hospitals: NITI Aayog
- 01 Oct 2021
- 6 min read
Why in News
Recently, NITI Aayog has released a performance assessment report of district hospitals in India, titled ‘Best Practices in the Performance of District Hospitals’.
Key Points
- About the Report:
- Collaboration: The report is an outcome of collaboration with the Ministry of Health and Family Welfare and WHO India.
- Data Validation: The National Accreditation Board for Hospitals and Healthcare Providers, a constituent board of the Quality Council of India, conducted the on-ground data validation.
- The Health Management Information System (HMIS) data for the year 2017–18 has been used as the baseline for this exercise.
- Categorisation: For this performance assessment, district hospitals were categorised into small (up to 200 beds), mid-sized (201-300 beds) and large hospitals (more than 300 beds).
- Of the total hospitals, 62% were small.
- Key Performance Indicators (KPIs): The assessment evaluated 707 district hospitals on 10 KPIs based on data from 2017-18.
- Number of functional hospital beds per 1,00,000 population
- Ratio of doctors, nursing staffs and paramedical staff in position to Indian Public Health Standards (IPHS) norm;
- Proportion of support services available
- Proportion of core health care services available
- Proportion of diagnostic services available
- Bed occupancy rate
- C-section rate
- Surgical productivity index
- OPD per doctor
- Blood bank replacement rate
- Key Findings:
- Beds per Population: On an average, a district hospital had 24 beds for 1,00,000 people.
- For the assessment, it was set that a hospital should have 22 beds for that many people (IPHS 2012 guidelines).
- The World Health Organization (WHO) recommends five hospital beds for every 1,000 people.
- Doctor-to-Bed Ratio: Only 27% of the total 707 districts assessed met the doctor-to-bed ratio of 29 doctors per 100 beds in a hospital.
- 88 hospitals out of 707 had the required ratio of staff nurses.
- Ratio of Paramedical Staff: Only 399 hospitals were found to have a ratio of paramedical staff in position as IPHS norms laid down (100 paramedical staff for 500 bed hospital).
- Support Services: On an average, every district hospital in India had 11 support services, compared to the required 14.
- Diagnostic Testing Services: Only 21 hospitals fulfilled the criteria of having all diagnostic testing services available.
- Bed Occupancy: 182 hospitals out of the 707 had bed occupancy of 90% or more.
- Occupancy of 80-85 % is considered ideal.
- OPD Patients: On an average, a doctor in a district hospital attends to 27 OPD patients.
- Beds per Population: On an average, a district hospital had 24 beds for 1,00,000 people.
- Suggestions:
- Increasing Resources: Adequate resources may be provided to district hospitals towards digitization.
- National and regional level training, workshops etc. may be organized to acknowledge as well as disseminate hospitals’ best practices.
- Linking with Medical Colleges: District hospitals may be linked to the nearest medical college by employing a hub and spoke distribution model, which is a cost-effective and time-saving transport and service distribution mechanism.
- Ensuring Optimal Resource Utilization: Ensuring 24×7 availability of support services, diagnostic testing facilities, pharmacy, and well-planned shifts of medical and paramedical staff would contribute to an optimal bed occupancy and resource utilization.
- Tele-medicine Services: Hospitals should encourage care seeking among the community through extension services, as also make seeking care a hassle-free and productive experience. Tele-medicine services can help increase OPD footfalls, with convenience to patients.
- Leveraging the ANM (Auxiliary Nurse Midwife)–ASHA–Anganwadi Worker (AAA) network, institutional deliveries over home deliveries should be encouraged and ensured.
- Increasing Resources: Adequate resources may be provided to district hospitals towards digitization.
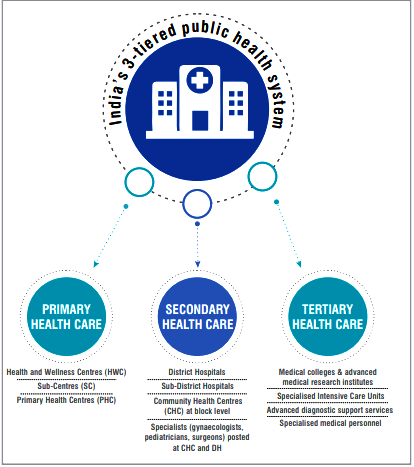
Public Healthcare in India
- Constitutional Provisions:
- Policy making in the country’s health sector is shaped by its federal structure and the Central-State divisions of responsibilities and financing.
- State List: Public health and sanitation, hospitals and dispensaries are state subjects, which means the primary responsibility of their management and service delivery lies with the states.
- Union List: The Centre also invests in health services through Centrally Sponsored Schemes such as the National Health Mission (NHM) and Ayushman Bharat.
- Concurrent List: The Centre plays an important role in vital statistics, medical education, and drugs administration, among others, which are subjects in the Concurrent List, as also in planning, policy making, and funding for public health at state and national levels.
- Policy making in the country’s health sector is shaped by its federal structure and the Central-State divisions of responsibilities and financing.
- Digitisation of Healthcare:
- National Digital Health Mission (NDHM): The NDHM is a complete digital health ecosystem. The digital platform will be launched with four key features: health ID, personal health records, Digi Doctor and health facility registry.
- Aarogya Setu App: It has an objective of enabling bluetooth based contact tracing and mapping of likely hotspots and dissemination of relevant information about Covid-19.
- National Health Policy 2017:
- The policy aims to achieve universal access to good quality health care services without anyone having to face financial hardship as a consequence.
- It intends to gradually increase public health expenditure to 2.5% of the GDP by 2025.
- It also envisages a three-dimensional integration of AYUSH systems encompassing cross referrals, co-location and integrative practices across systems of medicines.