Antimicrobial Resistance | 10 Jan 2024
For Prelims: National Centre for Disease Control (NCDC), Antimicrobial Resistance (AMR), World Health Organization (WHO), One Health Approach, Indian Council of Medical Research (ICMR).
For Mains: Antimicrobial Resistance, Government policies and interventions for development in various sectors and issues arising out of their design and implementation.
Why in News?
Recently, a survey conducted by the National Centre for Disease Control (NCDC) highlighted several key findings regarding the prescription and use of antibiotics in hospitals amidst growing concerns about Antimicrobial Resistance (AMR).
What are the Key Findings of the Survey?
- Preventative Use of Antibiotics:
- Over half of the surveyed patients (55%) were prescribed antibiotics for prophylactic indications, meant to prevent infections, rather than for therapeutic purposes (45%) to treat infections.
- Antibiotic Prescription Patterns:
- Only a small fraction (6%) of patients were prescribed antibiotics after a confirmed diagnosis of the specific bacteria causing their illness (definitive therapy), while the majority (94%) were on empirical therapy, based on the doctor’s clinical assessment of the likely cause of the illness.
- Lack of Specific Diagnosis:
- 94% of patients received antibiotics before a definitive medical diagnosis was confirmed, highlighting the prevalent use of antibiotics without precise knowledge of the infection's cause.
- Variation Among Hospitals:
- There were wide variations in antibiotic prescription rates among the hospitals, ranging from 37% to 100% of patients being prescribed antibiotics.
- A significant proportion (86.5%) of the prescribed antibiotics were administered through the parenteral route (not orally).
- Drivers of AMR:
- The NCDC survey notes, that one of the main drivers for the development of antibiotic resistance is the excessive and inappropriate use of antibiotics.
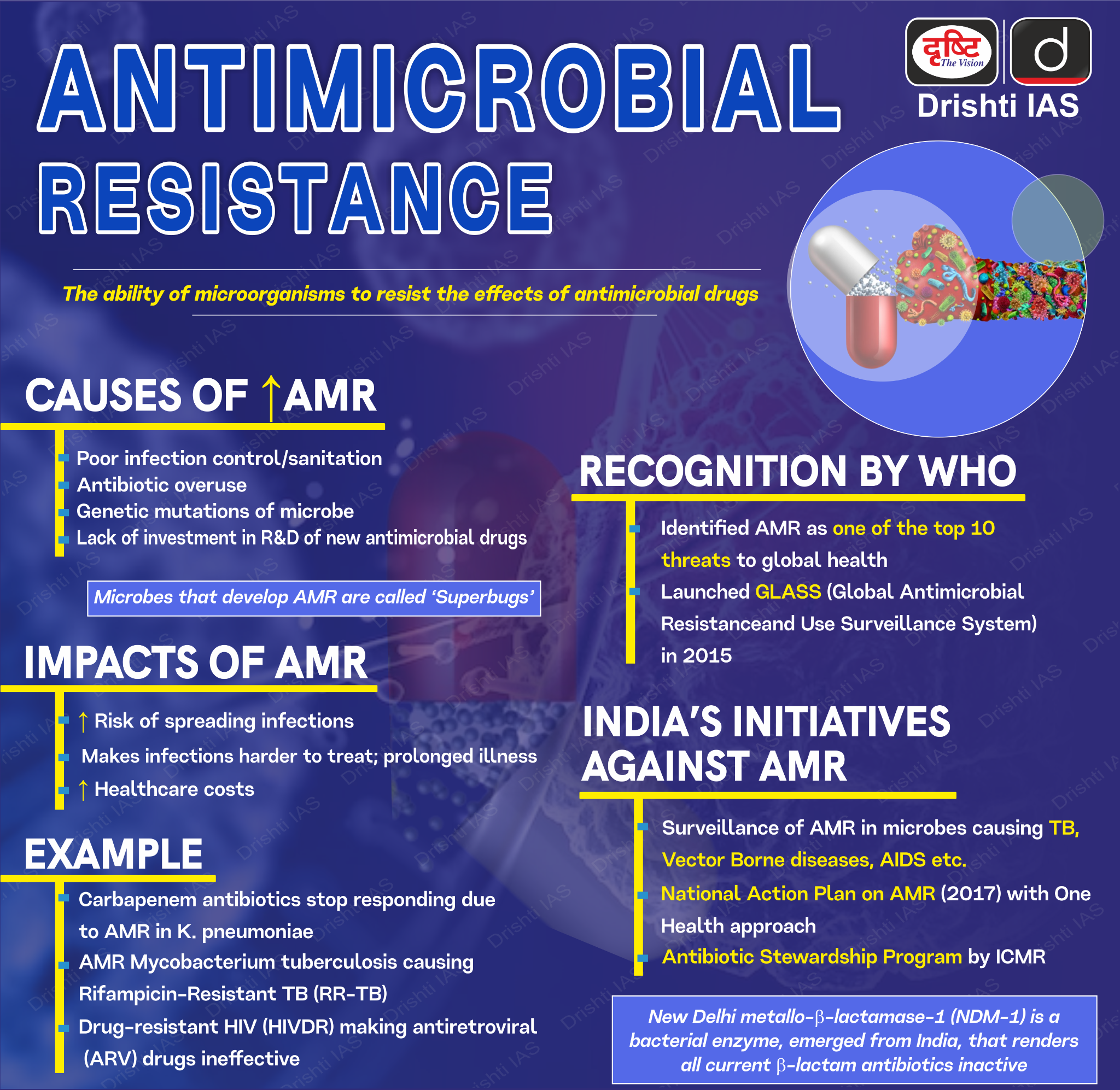
What is Antimicrobial Resistance (AMR)?
- About:
- Antimicrobial resistance is the resistance acquired by any microorganism (bacteria, viruses, fungi, parasites, etc.) against antimicrobial drugs (such as antibiotics, antifungals, antivirals, antimalarials, and anthelmintics) that are used to treat infections.
- As a result, standard treatments become ineffective, infections persist, and may spread to others.
- It is a natural phenomenon as bacteria evolve, making drugs used to treat infections less effective.
- Microorganisms that develop antimicrobial resistance are sometimes referred to as “superbugs”.
- The World Health Organization (WHO) has identified AMR as one of the top ten threats to global health.
- Antimicrobial resistance is the resistance acquired by any microorganism (bacteria, viruses, fungi, parasites, etc.) against antimicrobial drugs (such as antibiotics, antifungals, antivirals, antimalarials, and anthelmintics) that are used to treat infections.
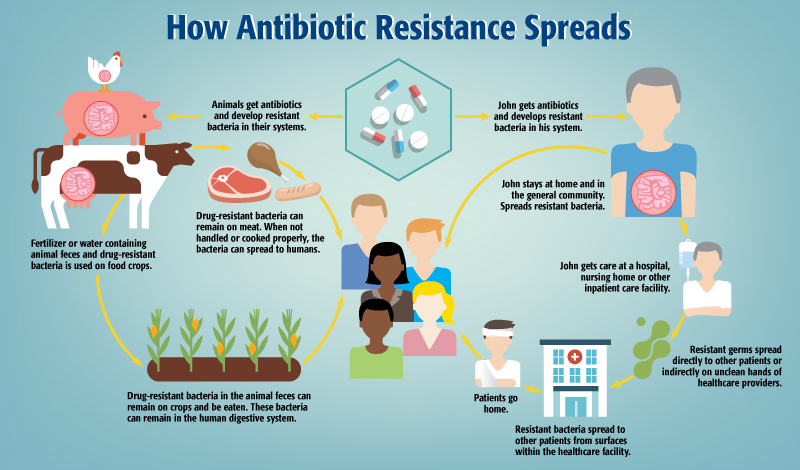
What are the Reasons for the Spread of AMR?
- High Prevalence of Communicable Diseases: High burden of communicable diseases, such as tuberculosis, diarrhoea, respiratory infections, etc. that require antimicrobial treatment.
- Overburdened Public Health System: This limits the laboratory capacity for etiology-based diagnosis and appropriately targeted treatment.
- Poor infection Control Practices: Hygiene lapses in hospitals and clinics facilitate the spread of resistant bacteria.
- Injudicious use: Overprescribing by doctors under pressure from patients (often self-medication), incomplete antibiotic courses, and broad-spectrum antibiotics used unnecessarily create selective pressure for resistant bacteria.
- Easy Access: Unregulated over-the-counter availability and affordability of antibiotics fuel self-medication and inappropriate use.
- Lack of Awareness: Low public understanding of AMR and proper antibiotic use encourages misuse.
- Limited Surveillance: Lack of adequate monitoring systems makes it difficult to track and understand the scope of AMR.
What are the Implications of the Spread of Antimicrobial Resistance?
- Healthcare Impact:
- AMR can render previously effective antibiotics ineffective against bacterial infections. This complicates the treatment of common illnesses like pneumonia, urinary tract infections, and skin infections, leading to prolonged illnesses, more severe symptoms, and increased mortality rates.
- Increased Healthcare Costs:
- Treating resistant infections often requires more expensive and prolonged therapies, increased hospital stays, and sometimes more invasive procedures. This leads to higher healthcare costs for individuals, healthcare systems, and governments.
- Challenges in Medical Procedures:
- AMR makes certain medical procedures riskier. Surgeries, cancer chemotherapy, and organ transplants become more hazardous due to the increased risk of infections that are resistant to standard antibiotics.
- Limitations in Treatment Options:
- As resistance grows, the available arsenal of effective antibiotics diminishes. This limitation in treatment options may lead to a scenario where previously manageable infections become untreatable, reverting medicine to a pre-antibiotic era where common infections could be fatal.
What are the Measures Taken to Address AMR ?
- Indian:
- National Programme on AMR containment: Launched in 2012. Under this programme, AMR Surveillance Network has been strengthened by establishing labs in State Medical College.
- National Action Plan on AMR: It focuses on One Health approach and was launched in April 2017 with the aim of involving various stakeholder ministries/departments.
- AMR Surveillance and Research Network (AMRSN): It was launched in 2013, to generate evidence and capture trends and patterns of drug resistant infections in the country.
- AMR Research & International Collaboration: Indian Council of Medical Research (ICMR) has taken initiatives to develop new drugs /medicines through international collaborations in order to strengthen medical research in AMR.
- ICMR along with Research Council of Norway (RCN) initiated a joint call for research in antimicrobial resistance in 2017.
- ICMR along with the Federal Ministry of Education and Research (BMBF), Germany has a joint Indo-German collaboration for research on AMR.
- Antibiotic Stewardship Program: ICMR has initiated antibiotic stewardship program (AMSP) on a pilot project across India to control misuse and overuse of antibiotics in hospital wards and ICUs.
- DCGI has banned 40 Fixed Dose Combinations (FDCs) which were found inappropriate.
- Global Measures:
- World Antimicrobial Awareness Week (WAAW): Held annually since 2015, WAAW is a global campaign that aims to raise awareness of AMR worldwide and encourage best practices among the general public, health workers and policymakers to slow the development and spread of drug-resistant infections.
- The Global Antimicrobial Resistance and Use Surveillance System (GLASS): WHO launched the GLASS in 2015 to continue filling knowledge gaps and to inform strategies at all levels.
- GLASS has been conceived to progressively incorporate data from surveillance of AMR in humans, surveillance of the use of antimicrobial medicines, AMR in the food chain, and the environment.
- Global Point Prevalence Survey Methodology: To deal with the challenge of limited information on how antibiotics are prescribed and used at the patient level, WHO has introduced the global point prevalence survey methodology to understand the prescribing patterns in hospitals, with repeated surveys showing the changes in antibiotic use over time.
- Few studies have been conducted in India using this methodology.
Way Forward
- Public Education Campaigns: Inform the public about AMR, its dangers, and how to prevent it. This can be done through mass media, community outreach programs, and educational materials in local languages.
- Antibiotic Stewardship Programs: Implement programs in hospitals and clinics to track and optimize antibiotic use, ensuring they are prescribed only when necessary and for the shortest effective duration.
- Regulation of Antibiotic Sales: Implement stricter regulations on the sale of antibiotics over the counter, requiring prescriptions for all antibiotics.
- Expand AMR Surveillance: Establish a nationwide AMR surveillance system to track the prevalence and spread of resistant bacteria in humans, animals, and the environment.
- Develop New Technologies: Explore the potential of new technologies, such as phage therapy, to address AMR challenges.
UPSC Civil Services Examination, Previous Year Questions (PYQ)
Prelims
Q. Which of the following are the reasons for the occurrence of multi-drug resistance in microbial pathogens in India? (2019)
- Genetic predisposition of some people
- Taking incorrect doses of antibiotics to cure diseases
- Using antibiotics in livestock farming
- Multiple chronic diseases in some people
Select the correct answer using the code given below.
(a) 1 and 2
(b) 2 and 3 only
(c) 1, 3 and 4
(d) 2, 3 and 4
Ans: (b)
Mains
Q. Can overuse and free availability of antibiotics without Doctor’s prescription, be contributors to the emergence of drug-resistant diseasesin India? What are the available mechanisms for monitoring and control? Critically discuss the various issues involved. (2014)