Combating Malnutrition in India
This editorial is based on the article “How to tackle malnutrition effectively” which was published in Indian Express on 29/01/2024. It talks about the prevalence of malnutrition in India and how to tackle it effectively.
For Prelims: Child Wasting, Stunting, National Family Health Survey 5 (NFHS 5), Mission Poshan 2.0, Integrated Child Development Services (ICDS) Scheme, Pradhan Mantri Matru Vandana Yojana (PMMVY), Mid-Day Meal Scheme, Scheme for Adolescent Girls (SAG), Mother’s Absolute Affection (MAA), Poshan Vatikas, Public Distribution System (PDS)
For Mains: Malnutrition, Severity of Malnutrition In India, Negative Consequences of Malnutrition in India, Key Challenges in Handling Malnutrition in India, Steps to Tackle Malnutrition in India
India faces a significant challenge with the prevalent burden of malnutrition. This issue is connected to the complicated mix of social, economic, and cultural differences in the country. The multifaceted nature of this pervasive problem demands urgent focus and dedicated resources to prevent a further decline in nutritional indicators.
What is Malnutrition?
- About Malnutrition:
- As per World Health Organization (WHO), malnutrition refers to deficiencies, excesses or imbalances in a person’s intake of energy and nutrients.
- It is a condition that arises from inadequate intake of vital nutrients essential for optimal health, growth, and development within an individual’s diet.
- Types:
- Undernutrition:
- Wasting: Low weight-for-height is known as wasting. It occurs when a person has not had enough food to eat and/or they have had an infectious disease.
- Stunting: Low height-for-age is known as stunting. It often occurs due to insufficient calorie intake, leading to a low weight for a given height.
- Underweight: Children with low weight-for-age are known as underweight. A child who is underweight may be stunted, wasted, or both.
- Micronutrient-related Malnutrition:
- Vitamin A Deficiency: Insufficient intake of vitamin A can lead to vision impairment, weakened immunity, and other health issues.
- Iron Deficiency: Causes anaemia, impacting the body's ability to transport oxygen, leading to fatigue and weakness.
- Iodine Deficiency: Results in thyroid-related disorders, affecting growth and cognitive development.
- Obesity: Excessive calorie intake, often coupled with a sedentary lifestyle, can lead to obesity. It is characterised by an accumulation of excess body fat, posing health risks like cardiovascular diseases and diabetes.
- In adults, overweight is defined as a Body Mass Index (BMI) of 25 or more, whereas obesity is a BMI of 30 or more.
- Diet-related Noncommunicable Diseases (NCDs): It encompasses cardiovascular diseases, such as heart attacks and strokes, often associated with high blood pressure, primarily stemming from unhealthy diets and inadequate nutrition.
- Undernutrition:
- Global Prevalence:
- Globally in 2022, 149 million children under 5 were estimated to be stunted (too short for age), 45 million were estimated to be wasted (too thin for height), and 37 million were overweight or obese.
- Nearly half of deaths among children under 5 years of age are linked to undernutrition.
- 1.9 billion adults are overweight or obese, while 462 million are underweight.
What is the Severity of Malnutrition in India?
- According to National Family Health Survey 5:
- Prevalence of Malnutrition:
- 35.5% of children under age five years are stunted
- 19.3% are wasted
- 32.1% are underweight
- 3% are overweight
- Malnutrition among women aged 15-49 years is 18.7%
- Prevalence of Anaemia:
- 25.0% in men (15-49 years)
- 57.0% in women (15-49 years)
- 31.1% in adolescent boys (15-19 yrs)
- 59.1% in adolescent girls
- 52.2% in pregnant women (15-49 years)
- 67.1% in children (6-59 months)
- Prevalence of Malnutrition:
- The State of Food Security and Nutrition in the World, 2023: Around 74% of India’s population could not afford a healthy diet, and 39% fell short of a nutrient-adequate one.
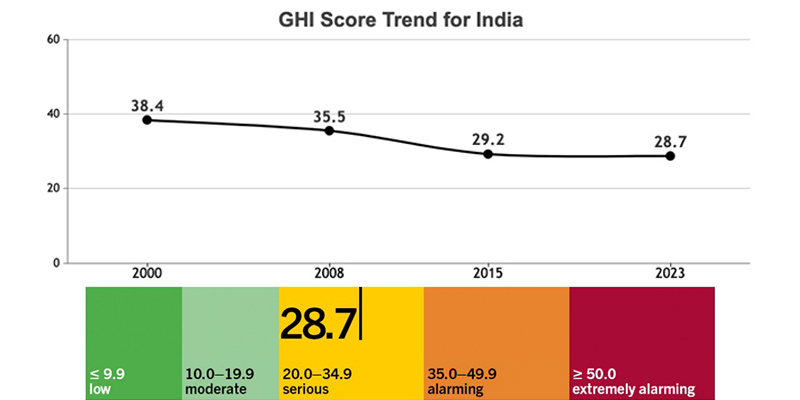
- According to Global Hunger Index 2023: India’s 2023 GHI score is 28.7, considered serious according to the GHI Severity of Hunger Scale.
- India's child wasting rate, at 18.7, is the highest child wasting rate in the report.
What are the Consequences of Malnutrition in India?
- Health Implications:
- Stunted Growth: Malnutrition, especially in children, can lead to stunted growth, impacting physical and cognitive development.
- Weakened Immune System: Malnourished individuals are more susceptible to infections due to a weakened immune system, leading to increased morbidity and mortality.
- Micronutrient Deficiencies: Consistent intake of micronutrient-lacking food can lead to deficiencies in iron, Vitamin A, and zinc, impairing immunity.
- Educational Consequences:
- Cognitive Impairment: Malnutrition during early childhood can affect cognitive function, hindering learning abilities and academic performance.
- School Dropout Rates: Malnourished children may face challenges in attending school regularly and are more likely to drop out, impacting their overall education.
- Economic Impact:
- Productivity Loss: Malnutrition can lead to decreased work productivity, both in childhood and adulthood, affecting the nation's overall economic output.
- Increased Healthcare Costs: The prevalence of malnutrition contributes to a higher burden on the healthcare system, leading to increased healthcare costs for the government and individuals.
- Inter-generational Impact:
- Maternal and Child Health: Anaemic mothers are more likely to give birth to anaemic babies, perpetuating the cycle of nutritional deficiencies.
- Long-term Health Effects: Malnourished children are more likely to face health challenges in adulthood, further impacting the overall health and well-being of the population.
- Social Consequences:
- Increased Vulnerability: Malnutrition often affects marginalised and economically disadvantaged communities, exacerbating social inequalities.
- Stigma and Discrimination: Individuals experiencing malnutrition may face societal stigma and discrimination, impacting their mental health and well-being.
- National Development:
- Reduced Human Capital: Malnutrition hampers the development of human capital, limiting the potential for economic and social progress.
- Increased Healthcare Burden: The prevalence of malnutrition contributes to an increased burden on healthcare resources, diverting attention and resources from other essential health initiatives.
What are Key Challenges in Handling Malnutrition in India?
- Economic Inequality: Due to the low economic status, poor people often cannot afford nutritious food or have limited access to it. They also face food insecurity due to natural disasters, conflicts, or price fluctuations.
- About 74% of India's population cannot afford a healthy diet.
- Inadequate Dietary Intake And Dietary Shifts: Dietary patterns have shifted from diverse and balanced options to processed and sugar-laden alternatives. The lack of dietary diversity and the consumption of low-quality food are also major contributors to malnutrition in India.
- The Indian diet is often deficient in essential nutrients such as Iron, Vitamin A, and Zinc.
- Poor Sanitation: Poor sanitation and hygiene practices can increase the exposure to pathogens and parasites that can cause infections and diseases. These can affect the absorption and utilisation of nutrients in the body and lead to malnutrition.
- The NFHS-5 found that only 69% of households use an improved sanitation facility.
- Lack of Primary Health Infrastructure: Many people in India do not have access to basic health services, such as immunisation, antenatal care, or treatment of infections. This increases the risk of diseases and complications that can worsen malnutrition.
- The WHO recommends a doctor to population ratio of 1 per 1000 and an ideal nurse density of 3 per 1000 people. In India, there are 0.73 doctors and 1.74 nurses per 1000 people.
- Delayed and Inconsistent Delivery: Delays in program implementation and inconsistent delivery of services contribute to gaps in nutritional interventions.
- According to the NFHS-5, only 50.3% of children under six years received any service from an Anganwadi.
- Inadequate Monitoring and Evaluation: Poor monitoring and evaluation mechanisms hinder the assessment of program effectiveness.
- Without accurate data on program outcomes, it becomes challenging to identify gaps and implement necessary improvements.
What Steps have been Taken by the Government of India Against Malnutrition?
How to Tackle Malnutrition in India Effectively?
- Adoption of Fortification: The addition of essential nutrients during the processing of staple foods is a relatively low-cost method, making it economically viable for large-scale implementation.
- Adoption of Iodised salt under the National Iodine Deficiency Disorders Control Programme in 1992 significantly reduced goitre rates.
- Develop a Focused SBCC Action Plan: The government should collaborate to develop a well-structured and focused Social and Behavior Change Communication (SBCC) Action Plan specifically tailored to address malnutrition.
- This plan should outline the objectives, target audience, key messages, and strategies for effective communication.
- Enhance Healthcare Infrastructure: The government shall take measures to strengthen healthcare facilities, especially in rural areas and to facilitate early detection and management of malnutrition.There should be more focus on improving the capacity of healthcare workers to diagnose and treat malnutrition.
- India needs 3.5 million additional hospital beds to adequately serve the healthcare needs of the population.
- National Health Policy recommended an increase in the Government’s health expenditure from the existing 1.2% to 2.5% of GDP by 2025.
- Monitoring and Evaluation: Establish robust monitoring and evaluation systems to track the impact of nutrition interventions.
- For instance, the Poshan Tracker records real-time data on malnourished and ‘severe acute malnourished’ children in each Anganwadi.
- Consumption of Locally Nutritious Food: The government should promote the consumption of locally available and traditional foods that are rich in essential nutrients. Encouraging consumption of a variety of locally available foods enhances dietary diversity.
- Community Empowerment: Involve local communities in designing and implementing nutrition programs. Establishing community-based initiatives will promote self-sufficiency in nutritious food production.
- Communication Strategies: Utilise communication channels like community radio, videos, and door-to-door outreach is essential to build trust among the beneficiaries
- Craft messages in vernacular languages to ensure better understanding and engagement, addressing local contexts.
Conclusion
To achieve the UN Sustainable Development Goal 2 of Zero Hunger by 2030 and eliminate malnutrition, India must prioritise and invest in the health and well-being of its population. Through a comprehensive and collaborative strategy, the nation can work towards significantly reducing malnutrition, unlocking the full potential of its people and fostering a healthier, more prosperous future.
|
Drishti Mains Question: Discuss the challenges posed by malnutrition in India. What effective measures can be implemented to combat malnutrition in the country? |
UPSC Civil Services Examination, Previous Year Question (PYQ)
Prelims:
Q. Which of the following is/are the indicators/ indicators used by IFPRI to compute the Global Hunger Index Report? (2016)
- Undernourishment
- Child stunting
- Child mortality
Select the correct answer using the code given below:
(a) 1 only
(b) 2 and 3 only
(c) 1, 2 and 3
(d) 1 and 3 only
Ans: C
Mains:
Q. How far do you agree with the view that the focus on lack of availability of food as the main cause of hunger takes the attention away from ineffective human development policies in India? (2018)