Social Issues
Mitigating TB Burden In India
This editorial is based on “TB control in India calls for person-centered solutions” which was published in The Hindu on 25/03/2024. The article discusses the persistent public health challenge posed by tuberculosis (TB) on a global scale and specifically in India. Despite India's health authorities setting ambitious goals for TB elimination, the progress has been slow, necessitating a carefully planned approach to effectively address this crisis.
For Prelims: Tuberculosis, Indian Council of Medical Research (ICMR), Nikshay Poshan Yojna, World Health Organization (WHO), Universal Health Coverage (UHC), United Nations (UN), TB Harega Desh Jeetega Campaign, National Strategic Plan (NSP) for Tuberculosis Elimination (2017-2025).
For Mains: Challenges to Eliminating TB, India’s Progress in Eliminating TB
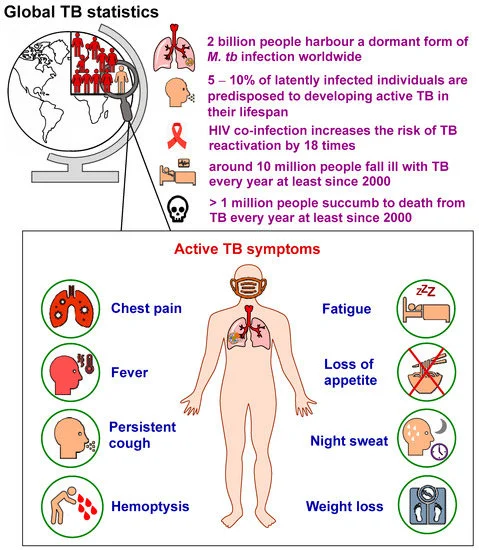
World TB Day, on March 24, commemorates Dr. Robert Koch’s discovery of Mycobacterium tuberculosis (the bacteria that causes tuberculosis) in 1882. Every day, 3,500 people worldwide lose their lives to tuberculosis (TB), and around 30,000 people become infected with TB bacilli, according to World Health Organization (WHO) estimates.
India alone accounts for 27% of global TB cases. This is astonishing, given that TB is a detectable and curable disease and TB diagnosis and treatment protocols have been a part of existing health systems for a long time.
Note
- Looking back, India’s fight against TB started even before independence:
- In 1929, India joined the International Union Against Tuberculosis. The King George V Thanksgiving Fund for TB control was established to support TB education and prevention, establish clinics, and train health workers.
- After independence in 1947, the Union government established a TB division under the Directorate General of Health Services with the Ministry of Health to oversee the plan.
- In 1959, the government, with the help of the WHO, established the National TB Institute in Bengaluru. Subsequently, the National Tuberculosis Control Programme (NTP) was formulated in 1962.
- The deficiency in the NTP was identified in 1963 and the Revised National TB Control Programme was developed. Fast forward to 2023, India’s National TB Elimination Programme is leading the effort to meet the goal of eliminating TB by 2025, five years ahead of the Sustainable Development Goals.
- Ending the TB epidemic by 2030 is among the health targets of the United Nations’ Sustainable Development Goals.
- In November 2023, the WHO acknowledged India’s success on two major fronts: in reducing TB incidence by 16% from 2015 to 2022 (close to double the pace at which global TB incidence is declining) and in reducing TB mortality by 18% during the same period, keeping in line with the global trend.
- Prime Minister addressed the One World TB Summit in Varanasi where he announced initiatives like TB Mukt Panchayat and roll-out of a shorter three-month course on preventive treatment towards achieving the goal of TB elimination by 2025.
- The PM also announced the nation-wide rollout of a 3-month preventive treatment for those at risk of developing TB. This will reduce the course of treatment from the previous six months and replace the daily pills with a once-a-week medicine regimen.
What is Tuberculosis (TB)?
- About:
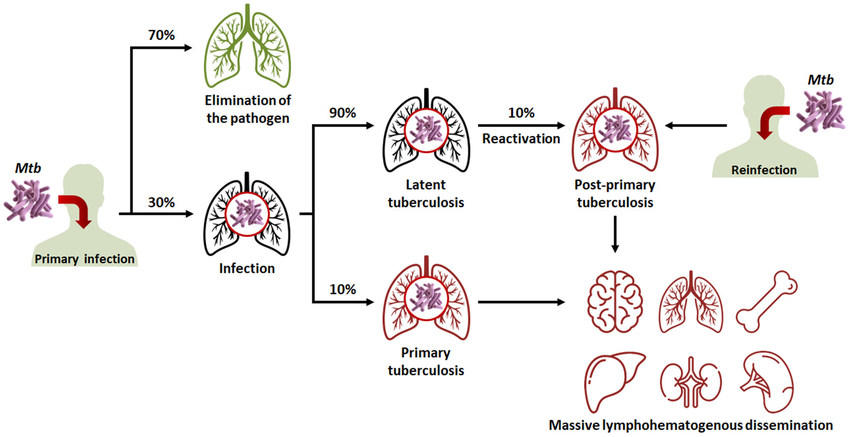
- TB is caused by a bacterium called Mycobacterium tuberculosis, belonging to the Mycobacteriaceae family consisting of about 200 members.
- Some of Mycobacteria cause diseases like TB and Leprosy in humans and others infect a wide range of animals.
- In humans, TB most commonly affects the lungs (pulmonary TB), but it can also affect other organs (extra-pulmonary TB).
- TB is a very ancient disease and has been documented to have existed in Egypt as early as 3000 BC. It is a treatable and curable disease.
- Infection Prevalence:
- Every year, 10 million people fall ill with TB. Despite being a preventable and curable disease, 1.5 million people die from TB each year – making it the world’s top infectious killer.
- TB is the leading cause of death of people with HIV and also a major contributor to antimicrobial resistance.
- Most of the people who fall ill with TB live in low- and middle-income countries, but TB is present all over the world. About half of all people with TB can be found in 8 countries: Bangladesh, China, India, Indonesia, Nigeria, Pakistan, Philippines and South Africa.
- Treatment:
- TB is treated with a standard 6-month course of 4 antimicrobial drugs that are provided with information, supervision and support to the patient by a health worker or trained volunteer.
- Anti-TB medicines have been used for decades and strains that are resistant to 1 or more of the medicines have been documented in every country surveyed.
- Multidrug-resistant tuberculosis (MDR-TB) is a form of TB caused by bacteria that do not respond to isoniazid and rifampicin, the 2 most powerful, first-line anti-TB drugs. MDR-TB is treatable and curable by using second-line drugs such as Bedaquiline.
- Extensively drug-resistant TB (XDR-TB) is a more serious form of MDR-TB caused by bacteria that do not respond to the most effective second-line anti-TB drugs, often leaving patients without any further treatment options.
What are the Different Issues in Curing TB Burden in India?
- Only Focussing on the Medical Aspect:
- The biggest deficiency has been in comprehending the real-life experiences of individuals affected by and battling TB. It is far too common for us to presume their requirements, difficulties, and anticipations.
- Occasionally, the system has erred by excessively medicalizing this illness, as is often the case with doctors and public health professionals.
- It has frequently failed to recognize TB as a humanitarian crisis, one with gender-specific implications, economic ramifications, and broader social and environmental impacts.
- Disproportionately Affecting Marginalised Section:
- While TB can affect people of any class, religion, ethnicity, and socioeconomic status, it disproportionately affects the most marginalised in society, including children, the urban poor, prisoners, and people living with HIV/AIDS.
- The disease has gone beyond being a health crisis alone. It is an economic crisis which by some estimates, costs India billions in losses each year and pushes families and communities into debt and poverty.
- Excessive Use of Antibiotics:
- Drug resistance in TB remains a man-made phenomenon. Unregulated use of antibiotics and non-compliance with treatment regimens lead to selective evolutionary pressure on the bacillus, in turn resulting in developing drug resistance.
- Poor regulatory mechanisms for drug control and non-compliance with treatment regimens are the main reasons for such a high degree of drug resistance.
- Assessing the Extent of Drug Resistant TB:
- There needs to be data on the proportion of people diagnosed with TB who have rifampicin-resistant TB (RR-TB) and multidrug-resistant TB (MDR-TB) - this is resistance to both rifampicin and isoniazid, collectively referred to as MDR/RR-TB.
- This helps in better plan and design of the control programme, resource allocation for diagnosis, the treatment regime as well as availability of trained staff mandated for DR-TB.
- There needs to be data on the proportion of people diagnosed with TB who have rifampicin-resistant TB (RR-TB) and multidrug-resistant TB (MDR-TB) - this is resistance to both rifampicin and isoniazid, collectively referred to as MDR/RR-TB.
- Reassessing the Screening Procedures:
- A Lancet study as well as the Indian Council of Medical Research’s ‘National TB Prevalence Survey in India’ showed that while screening people for symptoms is good, it is not substantive.
- Studies also show that in many cases, despite not showing any apparent symptoms, people may have infectious TB and may even be transmitting it. X-ray imaging is a quick and efficient way to find these patients.
- Tests Limited Due to High Cost and Accessibility Issues:
- The age-old sputum microscopy test has its limitations which are addressed by the newer molecular tests that are rapid, accurate, and even detect resistance against drugs. India has also scaled up molecular diagnostic capacity significantly.
- The NAAT (nucleic acid amplification test) machines in India have gone up from 651 in 2017 to more than 5,000 in 2022. But the utility of these tests is limited due to their high costs and issues with accessibility.
- The age-old sputum microscopy test has its limitations which are addressed by the newer molecular tests that are rapid, accurate, and even detect resistance against drugs. India has also scaled up molecular diagnostic capacity significantly.
- Challenges in Molecular Testing Reliant on Sputum Collection:
- First, It may not be as easy for everyone, especially young children, to produce sputum. Second, sample transportation, especially in remote and hilly districts, remains a challenge.
- During the COVID-19 pandemic, when an alternative to nasopharyngeal swabs was introduced in the form of simpler nasal swabs, saliva, and self-collection, the testing coverage greatly increased.
- First, It may not be as easy for everyone, especially young children, to produce sputum. Second, sample transportation, especially in remote and hilly districts, remains a challenge.
- Dual Burden of Diabetes Melitus (DM) and TB:
- DM increases the likelihood of unfavourable TB treatment outcomes, such as treatment failure, relapse/reinfection, and even death. The coexistence of TB and DM in patients may also modify TB symptoms, radiological findings, treatment, final outcomes, and prognosis.
- The dual burden of DM and TB not only impacts the health and survival of individuals but also places a significant burden on the healthcare system, families, and communities.
- DM increases the likelihood of unfavourable TB treatment outcomes, such as treatment failure, relapse/reinfection, and even death. The coexistence of TB and DM in patients may also modify TB symptoms, radiological findings, treatment, final outcomes, and prognosis.
What are the Steps to be Taken to Mitigate the TB Crisis?
- Prioritising the Needs and Interests of Patients and Communities:
- The needs and the interests of patients and communities must be prioritised within the care paradigm and the health-care system. This principle, echoed by survivors, communities, health experts and policymakers, underscores the need for a person-centred approach to TB care and management.
- Following a Individual-Centric Approach:
- The rise of influential advocates among TB survivors who have vigorously pushed for the inclusion of affected communities' needs in discussions. They have advocated for changes in various areas, leading governments to adjust their approaches to meet these community needs.
- For example, there has been some progress in providing nutritional support, albeit limited, which marks a significant advancement.
- The rise of influential advocates among TB survivors who have vigorously pushed for the inclusion of affected communities' needs in discussions. They have advocated for changes in various areas, leading governments to adjust their approaches to meet these community needs.
- Bridge the Gap Between Policy Intent and Ground Realities:
- There is a need to bridge the gap between policy intent and on-the-ground realities. For instance, India needs to prioritise targeted interventions aimed at improving and expanding access to TB diagnosis and treatment.
- TB testing facilities must be expanded, particularly in rural and underserved areas, and ensure the availability of free, affordable and quality-assured TB drugs.
- Molecular testing is the gold standard and less than a quarter of symptomatic patients are getting that as their first test.
- Making TB Care More Humane:
- Efforts are needed to strengthen community-based TB care models, empowering frontline health-care workers to deliver comprehensive care which addresses not just treatment but also social, economic and mental health needs and is closer to where patients live.
- This is important as survivor narratives tell us the stigma, discrimination and mental stress they go through, not to mention the side-effects of treatment.
- Adopting a Multi-Sectoral Approach:
- Addressing the socio-economic determinants of TB requires a multi-sectoral approach. Poverty alleviation, improvement in nutritional status, well-ventilated housing and better air quality will all contribute towards reducing TB.
- By tackling the underlying root causes of TB, India can make significant strides towards eliminating the disease and improving the overall health and well-being of its population.
- Tapping Technology:
- Leveraging technology and innovation holds promise in enhancing TB care efforts in India. The adoption of AI and digital health solutions for TB diagnosis, adherence and surveillance can revolutionise the way TB care is delivered and accessed in the country. By investing in developing better vaccines, we can hope to ultimately eliminate this airborne disease.
- X-ray technology has advanced dramatically. Now, we not only have portable hand-held devices, but also software driven by AI that can read digital X-ray images and detect possible TB with a high degree of certainty.
- Leveraging technology and innovation holds promise in enhancing TB care efforts in India. The adoption of AI and digital health solutions for TB diagnosis, adherence and surveillance can revolutionise the way TB care is delivered and accessed in the country. By investing in developing better vaccines, we can hope to ultimately eliminate this airborne disease.
- Implementing a 8-Point Agenda in Curing TB Burden:
- Early Detection: Given TB’s aetiology, early detection is the key. Symptoms are often ignored and mistaken for other common ailments, leading to delays in reporting. Compulsory screening for family and contacts of each index case is essential, necessitating availability of laboratory facilities and efficient follow-up mechanisms within health systems.
- Precise Treatment Categorisation: With increasing DR-TB, it is imperative to know the resistance status at the time of diagnosis to assign appropriate treatment regimens as per their phenotypic susceptibility.
- Treatment Adherence and Follow-Up: Unlike other bacterial diseases, TB requires a long period of sustained treatment. Often, this leads to non-compliance, which could be due to observable improvement in health status, or change of residence, movement across States and districts.
- Zero Mortality: Mitigating mortality due to TB, be it DR-TB or non-pulmonary TB, is necessary in order to realise the targets by 2025.
- Availability of Appropriate Medicines: Assured medical supply is mandated under the TB control programme. However, procurement challenges for DR-TB medications such as bedaquiline and delamanid must be addressed, in addition to ascertaining treatment facilities for all DR-TB cases which require in-patient care.
- Integration into Larger Health Systems: Strengthening referral networks within and between different levels of public health systems and private health systems is vital to ensure (a) no symptomatic cases are lost, (b) no patients miss their dosages and are non-compliant, and, importantly, (c) the screening of contacts for all positive cases of pulmonary TB cases (DR or non-DR).
- Dynamic Notification System: A robust notification system will ease the burden of health system personnel. While Ni-kshay has evolved — ‘Ni-Kshay-(Ni=End, Kshay=TB) is the web enabled patient management system for TB control under the National Tuberculosis Elimination Programme (NTEP)’ — it requires improvements to capture real-time TB data between sectors, practitioners, time, and locations.
- Considering Population Mobility and Migration: Often, the productive aspects of life are overlooked when discussing disease and health care seeking, particularly in the context of TB, which suffers from social and cultural stigma. Interestingly, once TB is diagnosed and positive cases are put on treatment, health is restored quickly for the patient to resume their daily activities. Therefore, portability of TB treatment within the country is crucial at the policy level.
What are Different Initiatives to Combat TB?
- Global Efforts:
- The WHO (World Health Organisation) has launched a joint initiative “Find. Treat. All. #EndTB” with the Global Fund and Stop TB Partnership.
- WHO also releases the Global Tuberculosis Report.
- India’s Efforts:
Conclusion
The path to TB elimination in India requires a concerted effort to prioritise person-centred care, address social determinants of health, and embrace innovation. By adopting a holistic and person-centred approach, India can overcome the barriers that stand in the way of TB control and create a healthier future for all its citizens.
There is a need to simply improve implementation and be more proactive in deploying new technologies. It is to be ensured that new technologies are streamlined and rolled out faster and capacity is built at the sub-district level to conduct diagnostic tests as needed.
|
Drishti Mains Question: Discuss the impact of tuberculosis (TB) on public health in developing countries, addressing challenges and strategies for prevention and control. |