Social Justice
Renewed Healthcare System
This article is based on India needs a renewed health-care system which was published in The Hindu on 19/07/2021. It talks about challenges of the public health care system in India and the ways forward.
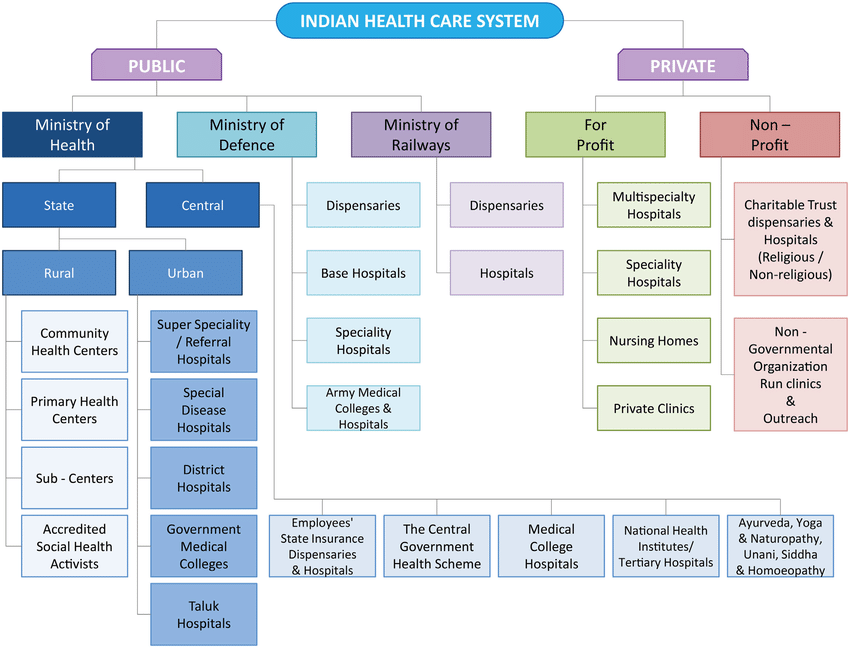
The Covid-19 pandemic reiterates the importance of Public Health systems. The private health sector which accounts for 70% of healthcare services in India, is playing only a supporting role.
There is a need to address the constraints and revamp of the public health system in India which would not only enable improved handling of Covid-19, but would also have widespread positive impacts extending much beyond the Covid-19 situation.
Covid-19 And Significance of Public Health Care
- For Indian population, the availability of functional public health systems is literally a question of life and death.
- A robust government health-care service is translated into a more effective outreach, timely testing, early case detection and more rational treatment for Covid patients. This is evident by comparing two States— Maharashtra and Kerala.
- Their per capita gross State domestic product (GSDP) is similar. However, their Covid-19 case fatality rates are hugely different — this being 0.48% for Kerala and 2.04% for Maharashtra.
- A major reason for such critical divergence is likely to be the huge differences in the effectiveness of public health systems.
- Kerala has per capita two and a half times more government doctors, and an equally higher proportion of government hospital beds when compared to Maharashtra, while allocating per capita over one and half times higher funds on public health every year.
- Despite Maharashtra having a large private health-care sector, its weak public health system has proved to be a critical deficiency.
Issues With Current Healthcare System
- Lack of Primary Healthcare Services: The existing public primary health care model in the country is limited in scope.
- Even where there is a well-functioning public primary health centre, only services related to pregnancy care, limited childcare and certain services related to national health programmes are provided.
- Supply-Side Deficiencies: Poor health management skills and lack of appropriate training and supportive supervision for health workers prevent delivery of the desired quality of health services.
- Inadequate Funding: Expenditure on public health funding has been consistently low in India (approximately 1.3% of GDP). As per OECD, India's total out-of-pocket expenditure is around 2.3 % of GDP.
- Sub-optimal Public Health System: Due to this, it is challenging to tackle Non-communicable Diseases, which is all about prevention and early detection.
- It diminishes preparedness and effective management for new and emerging threats such as pandemic like Covid-19.
Way Forward
- Focus On Public Health:
- Need for a larger programme which requires the immediate attention is the National Health Mission (NHM); since 2017-18, Union government allocations for the NHM have declined in real terms, resulting in inadequate support to States for core activities such as immunisation, while systemic gaps affect the delivery of Covid-19 vaccination.
- The condition of the National Urban Health Mission (NUHM) also remains pathetic.
- This year’s Central allocation for the NUHM is ₹1,000 crore, which amounts to less than ₹2 per month per urban Indian.
- Private Sector Regulation:
- Another clear priority that has been highlighted during the Covid-19 pandemic is the need to regulate rates and standards of care in the private sector.
- Massive hospital bills have caused untold distress even among the middle class.
- Although various determinants have contributed to the Mucormycosis outbreak, irrational use of steroids in Covid-19 patients, especially diabetics, appears to be an important factor.
- The central government should take necessary steps to promote the implementation of the Clinical Establishments (Registration and Regulation) Act (CEA).
- Passed in 2010 and presently applicable to 11 States across India, this Act is not effectively implemented due to a major delay in notification of central minimum standards, and failure to develop the central framework for regulation of rates.
- NITI Aayog Prescriptions:
- NITI Aayog has recently published the document, ‘Investment Opportunities in India’s Healthcare Sector’.
- The document states that ‘in the hospital segment, the expansion of private players to Tier 2 and Tier 3 locations, beyond metropolitan cities, offers an attractive investment opportunity’.
- Manufacturing of medical devices and equipment, expansion of diagnostic and pathology centres and miniaturized diagnostics have high growth potential.
- Technology advancements such as Artificial Intelligence, wearables and other mobile tech, along with the Internet of Things, also offer numerous avenues for investment.
Conclusion
Existing evidence from the Covid-19 pandemic provides a clear message that a neglect of public health systems can mean large-scale, avoidable losses of lives; hence, public health services must be upgraded rapidly and massively as a topmost priority.
|
Drishti Mains Question The Covid-19 pandemic highlights issues and reiterates the importance of Public Health systems. Comment. |