Governance
Tackling Sickle Cell Disease in India
This editorial is based on “India’s Sickle Cell Challenge” which was published in The Hindu on 12/09/2024. The article highlights the key challenges associated with sickle cell disease in India and proposes strategies to address these issues effectively.
For Prelims: Sickle Cell Disease (SCD), Red blood cells (RBCs), Chronic anaemia, Lyfgenia, CRISPR, National Sickle Cell Anaemia Elimination Mission, National Health Mission (NHM) 2013, Rights of Persons with Disabilities (RPwDs) Act, 2016, SDG 3.
For Mains: Prevalence of Sickle Cell Disease in India, Key challenges encountered by the SCD Healthcare System in India, Steps needed to effectively combat the SCD in India.
Last year, the Prime Minister of India launched the National Sickle Cell Anaemia Elimination Mission from Shahdol, Madhya Pradesh, setting an ambitious target to eradicate sickle cell disease (SCD) as a public health threat by 2047. SCD disproportionately impacts India's tribal and rural communities, where it remains a longstanding and urgent challenge.
Despite advancements in SCD healthcare, sickle cell disease continues to be significantly underdiagnosed and poorly managed in many regions, underscoring the need for more comprehensive action.
What is Sickle-Cell Disease (SCD)?
- About:
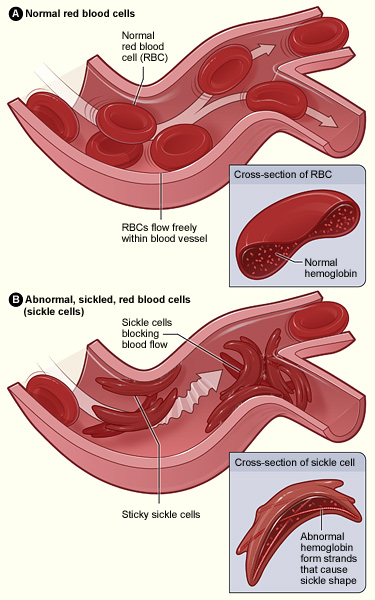
- Sickle Cell Disease (SCD) is an inherited hemoglobin disorder characterized by a genetic mutation that causes red blood cells (RBCs) to assume a sickle or crescent shape rather than their normal round shape.
- The lifespan of patients with sickle cell disease is significantly reduced, averaging around 40 years.
- Their quality of life is severely affected by a range of health complications, including sickle cell anemia, recurrent infections, persistent pain, swelling, and damage to vital organs
- Individuals with SCD suffer from both acute and chronic complications, which include recurring episodes of pain commonly called vaso-occlusive crisis (VOC) - acute chest syndrome (ACS), aseptic necrosis of bone, micro infarction of spleen, brain, and kidney, infections, stroke, and organ damage affecting every organ in the body.
- Causes :
- SCD is a genetic condition that is present at birth. It is inherited when a child receives two genes—one from each parent—that code for abnormal hemoglobin.
- Common Types :
- The specific type of SCD a person has depends on the genes they inherited from their parents. People with SCD inherit genes that contain instructions, or code, for abnormal hemoglobin.
- HbSS: People who have this form of SCD inherit two genes, one from each parent, that code for hemoglobin "S."
- HbSC: People who have this form of SCD inherit a hemoglobin S gene from one parent and a gene for a different type of abnormal hemoglobin called "C" from the other parent. This is usually a milder form of SCD.
- HbS beta thalassemia: People who have this form of SCD inherit a hemoglobin S gene from one parent and a gene for beta thalassemia, another type of hemoglobin abnormality, from the other parent.
- HbSD, HbSE, and HbSO : People who have these forms of SCD inherit one hemoglobin S gene and one gene that codes for another abnormal types of hemoglobin ("D," "E," or "O").
- The specific type of SCD a person has depends on the genes they inherited from their parents. People with SCD inherit genes that contain instructions, or code, for abnormal hemoglobin.
- Symptoms: Symptoms of sickle cell disease can vary, but some common symptoms are-
- Chronic anaemia which leads to fatigue, weakness, and paleness.
- Painful episodes (also known as sickle cell crisis) cause sudden and intense pain in the bones, chest, back, arms, and legs.
- Delayed growth and puberty.
- Treatment Processes:
- Blood Transfusions: These can help relieve anaemia and reduce the risk of pain crises.
- Hydroxyurea: This medication can help reduce the frequency of painful episodes and prevent some of the disease's long-term complications.
- Gene Therapy: It can also be treated by bone marrow or stem cell transplantation by methods like Clustered regularly interspaced short palindromic repeats (CRISPR).
What is the Prevalence of Sickle Cell Disease in India ?
- Public Health Concern: The Ministry of Health and Family Welfare (MoHFW) has recognized sickle cell disease (SCD) as one of the ten major health issues disproportionately impacting India's tribal population.
- Global Burden: India bears the world’s second-largest burden of SCD, with over 1 million people affected by the disease.
- SCD Birth Rates: India ranks third globally in the number of SCD births, following Nigeria and the Democratic Republic of the Congo.
- Carrier Rate: The prevalence of sickle cell carriers among different tribal groups varies from 1 to 40%.
- Geographical Distribution:
- The majority of SCD patients are concentrated in the tribal belt that spans across Odisha, Jharkhand, Chhattisgarh, Madhya Pradesh, and Maharashtra.
What are the Key Challenges Encountered by the SCD Healthcare System in India?
- No Permanent Cure : There is currently no permanent cure for sickle cell disease.
- While ongoing research into gene therapy shows promise, it is likely to remain unaffordable for most of the affected population even once it becomes available.
- Misdiagnosis : Getting an accurate diagnosis is challenging because many individuals are reluctant to seek help due to the stigma surrounding the condition.
- As a result, they often turn to traditional healers, who frequently misdiagnose the disease.
- Inadequate Healthcare Infrastructure: Many rural and tribal areas lack specialised healthcare facilities and trained medical personnel for managing SCD.
- This hampers timely intervention and effective disease management.
- Inadequate Screening Programs: The absence of systematic newborn screening and early detection initiatives results in missed opportunities for early intervention and genetic counseling.
- There is mistrust of public healthcare in tribal areas, leading to low testing rates.
- Limited Access to Medications:Medicines like Hydroxyurea are effective but access to medications is inconsistent, with stockouts and long travel distances for patients.
- Only 18% of the people affected by sickle cell disease in India are receiving consistent treatment.
- High Treatment Costs: The long-term management of SCD can be financially burdensome for many families due to the cost of medications, regular check-ups, and potential hospitalizations.
- Treatments like CRISPR cost $ 1-2 million, and it's difficult to find bone marrow donors.
- Inadequate Research and Data: Limited research on SCD, particularly in the context of India’s diverse populations, hinders the development of effective treatment strategies and public health interventions tailored to local needs.
- Cultural and Social Barriers: Stigma and social attitudes toward SCD can discourage individuals from seeking treatment or participating in screening programs, affecting overall health outcomes.
What are the Government Initiatives Regarding SCD?
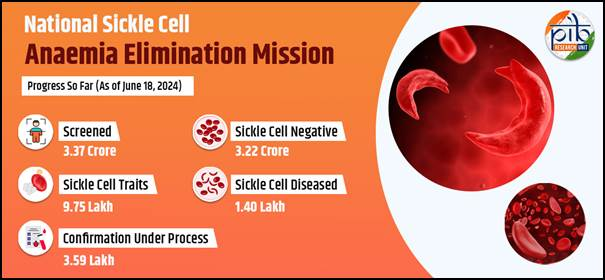
- National Sickle Cell Anaemia Elimination Mission:
- Aimed at enhancing the care for all Sickle Cell Disease (SCD) patients and reducing the disease's prevalence through an integrated approach encompassing screening and awareness campaigns.
- Targeting complete elimination of sickle cell disease as a public health concern by 2047.
- Under the Sickle Cell Anaemia Mission, the Council of Scientific and Industrial Research (CSIR) is developing gene-editing therapies for SCD.
- National Health Mission (NHM) 2013:
- It is, a flagship programme of the Indian government, that encompasses provisions for disease prevention and management, with a specific focus on hereditary anomalies such as sickle cell anaemia.
- Dedicated programs within NHM focus on raising awareness, facilitating early detection, and ensuring timely treatment of sickle cell anaemia.
- NHM facilitates drugs like hydroxyurea to treat SCD in its “essential medicines List”.
- The National Guidelines for Stem Cell Research 2017:
- It restricts the commercialisation of stem cell therapies to clinical trials, except for Bone marrow transplantation (BMT) for SCD.
- Gene editing on stem cells is permitted only for in-vitro studies.
- National Guidelines for Gene Therapy Product Development and Clinical Trials 2019: It provides guidelines for the development and clinical trials of gene therapies for inherited genetic disorders.
- India has also approved a five-year project to develop CRISPR techniques for sickle cell anaemia treatment.
- State Haemoglobinopathy Mission of Madhya Pradesh:
- It aims to address the challenges in screening and management of the disease.
- Rights of Persons with Disabilities (RPwDs) Act, 2016:
- SCD is included in the 21 disabilities that provide for benefits such as reservation in higher education (minimum 5%), government jobs (minimum 4%), and allocation of land (minimum 5%), for persons with benchmark disabilities and those with high support needs.
- Free education is guaranteed for every child with a benchmark disability between 6 and 18 years.
Note
- Recently, the US Food and Drug Administration (FDA) approved two gene therapies designed for sickle cell disease.
- The approved therapies include Lyfgenia and Casgevy.
- Both treatments received clearance for individuals aged 12 years and above.
- Casgevy also approved in the U.K., is the first CRISPR-based therapy to have received regulatory approval.
- Lyfgenia doesn’t use CRISPR but depends on a viral vector to change blood stem cells.
- Both treatments entail collecting a patient’s blood stem cells, modifying them, and administering high-dose chemotherapy to destroy the damaged cells in the bone marrow.
- The modified cells are then infused into the patient through a hematopoietic stem cell transplant.
What Steps Should be Taken to Effectively Combat the Disease?
- Reduce Stigma and Foster Trust :
- To combat sickle cell disease effectively, it is essential to reduce stigma and foster trust in public health institutions.
- India can leverage its successful strategies from past health campaigns, such as those against polio and HIV, to raise awareness and educate the public.
- Early Detection and Screening:
- Given that cases are often missed and diagnoses delayed, increasing newborn screening could be crucial.
- Strengthen and expand genetic counseling and testing programmes.
- Prioritising basic treatments like hydroxyurea is essential for urgent needs.
- Enhancing Accessibility to Care :
- Drugs and adherence support must be readily available at local health and wellness centers.
- To manage complications, interdisciplinary centers of excellence should be established and operational at the district or divisional level.
- Implementing Catch-Up Vaccination Programs :
- Ensuring that all known patients receive approved vaccines is crucial and may necessitate the implementation of catch-up vaccination programs.
- Research and Development:
- Allocate more resources for ongoing medical research.
- Gain deeper insights into the genetic and molecular aspects of SCD to develop more effective treatment options and potential cures.
- For this, philanthropists and civil society members must take on a catalytic role, collaborating closely with Central and State governments.
Conclusion
Addressing sickle cell disease in India by enhancing early detection, healthcare infrastructure, and public education supports SDG 3 (Good Health & Well Being) and SDG 10 (Reduced Inequality). Through sustained commitment and coordinated efforts, it is possible to transform the landscape of sickle cell disease management in India, ultimately improving health outcomes and reducing the suffering associated with this debilitating condition.
|
Drishti Mains Question: Discuss the extent of the sickle cell disease burden in India and propose effective strategies to tackle it. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q.Which one of the following statements best describes the role of B cells and T cells in the human body? (2022)
(a) They protect the body from environmental allergens.
(b) They alleviate the body’s pain and inflammation.
(c) They act as immunosuppressants in the body.
(d) They protect the body from the diseases caused by pathogens.
Ans: D
Mains
Q.Stem cell therapy is gaining popularity in India to treat a wide variety of medical conditions including Leukaemia, Thalassemia, damaged cornea and several burns. Describe briefly what stem cell therapy is and what advantages it has over other treatments? (2017)