Governance
Striving for a Future Without Cervical Cancer
This editorial is based on “ A bold step towards a cervical cancer-free future” which was published in The Hindu on 08/03/2024. The article delves into the necessity and obstacles faced by the HPV vaccination program aimed at eliminating cervical cancer in the country.
For Prelims: Cervical Cancer, HPV strains, Human Papillomavirus(HPV), Sustainable Development Goals(SDGs), National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke, National Cancer Awareness Day, National Cancer Grid, CERVAVAC
For Mains: Requirements and Hurdles in Combating Cervical Cancer in India.
Cervical Cancer continues to pose a substantial health threat in India, emphasizing the necessity of preventive measures. The Government of India intends to initiate a three-phase vaccination drive against Human Papillomavirus (HPV) for girls aged 9-14, aiming to mitigate the risk of cervical cancer.
However, understanding the risk factors, vaccination options, screening protocols, and management of precancerous conditions is crucial to effectively combat this preventable disease.
What is Cervical Cancer?
- About:
- Cervical Cancer develops in a woman's cervix. It is the 4th most common type of cancer among women, globally.
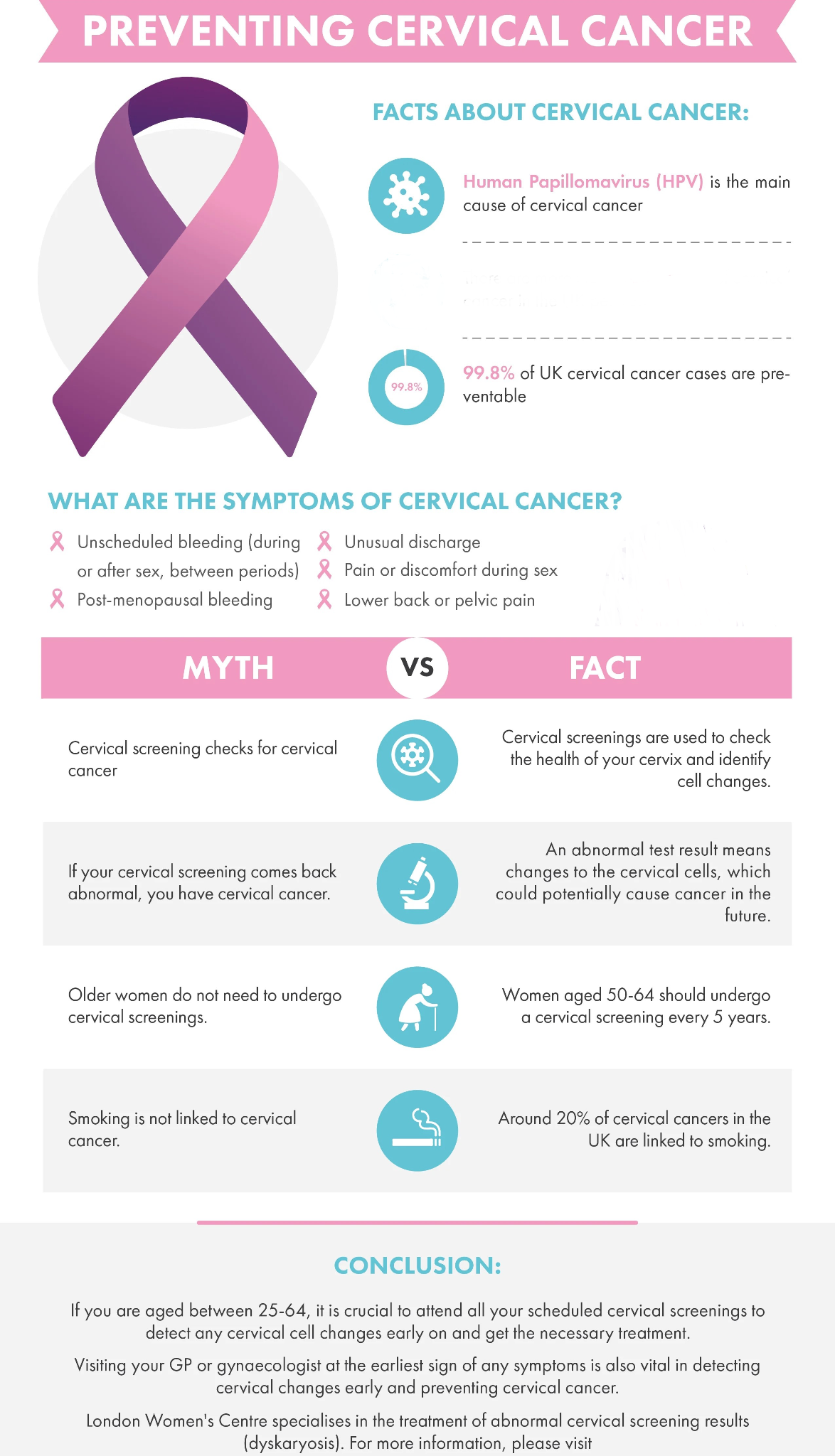
- Almost all cervical cancer cases (99%) are linked to infection with high-risk Human Papillomavirus (HPV), an extremely common virus transmitted through sexual contact.
- Types of Strain:
- Persistent infections with certain high-risk HPV strains lead to nearly 85% of all cervical cancers.
- At least 14 HPV types have been identified as oncogenic (potential to cause cancer).
- Among these, HPV types 16 and 18, considered to be the most oncogenic, have been found to be responsible for about 70% of all cervical cancer cases globally.
Why Fighting with Cervical Cancer is Crucial for India?
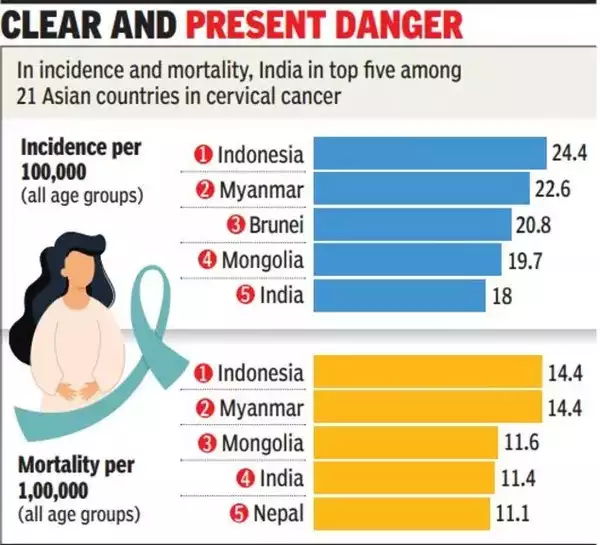
- High Prevalence and Mortality Rates: Cervical cancer ranks as the second most common cancer among women in India, with approximately 1.27 lakh cases reported annually and contributing to around 80,000 deaths each year.
- Comorbidities and Risk Factors: Human papillomavirus (HPV) infection, primarily transmitted through sexual contact, is a leading cause of cervical cancer in India.
- The high prevalence of comorbidities like HIV/AIDS and risk factors such as early marriage, multiple sexual partners, and lack of contraception use further complicate efforts to eradicate cervical cancer.
- Disproportionate Impact on Underserved Communities: Cervical cancer disproportionately affects women in underserved and marginalized communities due to limited access to healthcare facilities, inadequate awareness, and socio-economic factors.
- Economic Burden: The economic burden of cervical cancer is significant, with costs associated with diagnosis, treatment, and care straining healthcare resources and exacerbating financial hardships for affected individuals and their families.
- Impact on Women's Well-being: Cervical cancer predominantly affects women during their prime years, leading to premature deaths that impact families' socio-economic stability and children's well-being.
- Human Rights Issue: Access to affordable and quality healthcare services, including HPV vaccination and cervical cancer screening, is essential for fulfilling women's right to health and well-being.
- Long-term Benefits: Investing in cervical cancer prevention and control efforts yields long-term benefits for public health and sustainable development, contributing to improvements in life expectancy, maternal and child health outcomes, and progress toward achieving the Sustainable Development Goals(SDGs).
What Obstacles Hinder the Eradication of Cervical Cancer in India?
- Limited Awareness: Many individuals, particularly in rural and underserved areas, lack awareness about cervical cancer, its risk factors, and preventive measures like HPV vaccination and regular screening.
- Inadequate Screening Programs: There is a lack of widespread and accessible cervical cancer screening programs in India, leading to late-stage diagnoses and poor treatment outcomes.
- Lack of Access to Formal Health Care: Insufficient healthcare infrastructure, particularly in rural areas, hinders early detection, diagnosis, and treatment of cervical cancer.
- A study in Andhra Pradesh revealed that 68% of patients first sought traditional healers, and only 3% had received HPV vaccination.
- Shortage of Skilled Personnel: There is a shortage of skilled healthcare professionals, including gynecologists and oncologists, trained in cervical cancer prevention, screening, and treatment.
- Stigma and Cultural Barriers: Sociocultural taboos surrounding women's health issues, including cervical cancer, may prevent women from seeking timely medical care or participating in screening programs.
- Vaccine Hesitancy: Misinformation and misconceptions about HPV vaccination contribute to vaccine hesitancy among parents and caregivers, affecting vaccination coverage rates.
- Affordability and Accessibility: The cost of HPV vaccines, screening tests, and treatment options may be prohibitive for many individuals, particularly those from low-income backgrounds.
- Geographic Disparities: Cervical cancer incidence and mortality rates vary significantly across different regions of India, with rural areas often experiencing higher disease burdens and fewer healthcare resources.
- Limited Government Funding: Insufficient funding for cervical cancer prevention and control programs hampers efforts to implement comprehensive strategies and interventions.
- Limited Research and Innovation: More research and innovation are needed to develop affordable and effective screening tools, diagnostic techniques, and treatment modalities tailored to the Indian context.
What are the Government Initiatives Related to Cancer Treatment?
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke
- National Cancer Grid
- National Cancer Awareness Day
- HPV Vaccine
- Government Initiatives for Cancer Screening: The Government of India implements cancer screening, including visual tests and HPV tests, in primary health centres.
How India Can Battle the Menace of Cervical Cancer?
- HPV Vaccination:
- Persistent high-risk HPV infection, along with factors like low socioeconomic conditions and smoking, leads to cervical cancer.
- Through HPV vaccination, screening, and timely treatment can prevent and cure the disease.
- Persistent high-risk HPV infection, along with factors like low socioeconomic conditions and smoking, leads to cervical cancer.
- Opportunity for Early Detection and Treatment:
- Cervical cancer has a 10–15 year pre-invasive phase, offering a window for early detection and outpatient treatment.
- Early-stage management yields a cure rate exceeding 93%, highlighting the importance of timely interventions.
- Cervical cancer has a 10–15 year pre-invasive phase, offering a window for early detection and outpatient treatment.
- Indigenous Vaccine Development:
- India's milestone in developing the indigenous quadrivalent vaccine, Cervavac, promises accessibility and affordability.
- CERVAVAC is India’s first indigenously developed quadrivalent human papillomavirus (qHPV) vaccine that is said to be effective against four strains of the virus - Type 6, Type 11, Type 16 and Type 18.
- Priced at ₹2,000 a dose, Cervavac holds promise in the fight against HPV infections and cervical cancer.
- Draw Lessons from the Global Success of HPV Vaccination:
- Over 100 countries globally have implemented successful HPV vaccination programs, leading to a notable decline in cervical cancer cases.
- Studies from Scotland and Australia demonstrate the real-world impact of HPV vaccines, with significant reductions in cervical cancer incidence.
- Rwanda's successful HPV vaccination campaign underscores the importance of prioritizing vaccination for combating cervical cancer.
- '90-70-90' Targets by WHO: The World Health Organization has set ambitious targets aiming for 90% of girls to be fully vaccinated with the HPV vaccine by age 15, 70% of women to undergo cervical cancer screening tests by the ages of 35 and 45, and for 90% of women with cervical cancer to receive treatment by 2030.
- Role of Technological Advancements:
- Innovations like single-dose HPV vaccination, self-sampling for HPV testing, and Artificial Intelligence (AI) technologies enhance cervical cancer prevention.
- These developments, along with increased HPV vaccine uptake, hold promise for resource-limited settings.
- Innovations like single-dose HPV vaccination, self-sampling for HPV testing, and Artificial Intelligence (AI) technologies enhance cervical cancer prevention.
- Population-Level Awareness and Strategies:
- Addressing cervical cancer requires increasing awareness, promoting HPV vaccine uptake, overcoming hesitancy, implementing age-appropriate screening, and strengthening pre-cancer treatment processes.
- Including HPV information in health education in schools can be a step to generate demand among adolescents.
Conclusion
The alarming statistics of new cases and deaths highlight the urgent need for preventive measures. Early detection through screening and HPV vaccination presents a crucial opportunity, with a high cure rate when managed at early stages. There is a need for consistent and coherent efforts for accurate diagnosis, strengthened cancer registries, reduced financial burden, and robust health systems for the successful elimination of cervical cancer.
|
Drishti Mains Question : Examine the urgency of fighting cervical cancer in India, consider the challenges involved, and propose measures to address them. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims:
Q1. ‘Mission Indradhanush’ launched by the Government of India pertains to (2016)
(a) Immunization of children and pregnant women
(b) Construction of smart cities across the country
(c) India’s own search for the Earth-like planets in outer space
(d) New Educational Policy
Ans: A
Mains:
Q1.What are the research and developmental achievements in applied biotechnology? How will these achievements help to uplift the poorer sections of the society ? (2021)