ART’s Intervention in HIV/AIDS Treatment
This editorial is based on “The ART of India’s HIV/AIDS response” which was published in The Hindu on 01/04/2024. The article explores the role of Antiretroviral Therapy (ART) in managing HIV/AIDS and the insights it offers for other public health initiatives.
For Prelims: Acquired Immunodeficiency Syndrome (AIDS), Human Immunodeficiency Virus (HIV), Antiretroviral Therapy (ART).
For Mains: Challenges Related to AIDS), Significance of Antiretroviral Therapy (ART).
April 1, marks a very important day in the history of response to the HIV/AIDS epidemic in India. Twenty years ago, on April 1, 2004, the Indian government had launched Antiretroviral Therapy (ART), for Persons living with HIV (PLHIV), a decision which has proven one of the successful and a key intervention in the fight against HIV/AIDS.
What is HIV/AIDS?
- About:
- HIV/AIDS is a viral infection that attacks the immune system, specifically the CD4 cells (T cells), which help the immune system fight off infections.
- Left untreated, HIV reduces the number of CD4 cells (T cells) in the body, making the person more likely to get infections or infection-related cancers.
- AIDS is the final stage of HIV infection, when the immune system is severely damaged and can no longer fight off infections.
- Causes of HIV/AIDS:
- HIV infection is caused by the human immunodeficiency virus (HIV). The virus is transmitted through contact with infected bodily fluids, such as blood, semen, vaginal fluids, rectal fluids, and breast milk.
- It can be spread through sexual contact, sharing needles or syringes, from mother to child during childbirth or breastfeeding, and rarely, through blood transfusions or organ transplants.
- Symptoms of HIV/AIDS:
- Acute HIV Infection:
- Symptoms can resemble those of the flu, including fever, swollen lymph nodes, sore throat, rash, muscle and joint aches, and headache.
- Clinical Latent Infection:
- HIV is still active but reproduces at very low levels. People may not have any symptoms or only mild ones.
- AIDS:
- The symptoms of AIDS are severe and include rapid weight loss, recurring fever or profuse night sweats, extreme and unexplained tiredness, prolonged swelling of the lymph glands in the armpits, groin, or neck, diarrhoea that lasts for more than a week, sores of the mouth, anus, or genitals, pneumonia, and red, brown, pink, or purplish blotches on or under the skin or inside the mouth, nose, or eyelids.
- Acute HIV Infection:
- Diagnosis of HIV/AIDS:
- HIV antibody/antigen tests: These tests detect antibodies or antigens produced by the virus and are usually done on blood or oral fluid.
- Nucleic acid tests (NATs): These tests look for the virus itself and can detect HIV infection earlier than antibody tests.
- Treatment and Management:
- Antiretroviral therapy (ART): ART involves taking a combination of HIV medicines every day. ART can't cure HIV, but it can control the virus, allowing people with HIV to live longer, healthier lives and reducing the risk of transmitting the virus to others.
- Pre-exposure prophylaxis (PrEP): PrEP is a daily pill for people who don't have HIV but are at risk of getting it. When taken consistently, PrEP can reduce the risk of HIV infection.
What is Antiretroviral Therapy (ART)?
- About:
- Antiretroviral therapy (ART) is a cornerstone treatment for managing HIV/AIDS, a chronic viral infection caused by the human immunodeficiency virus (HIV).
- This therapy aims to suppress the replication of HIV in the body, thereby reducing viral load, preserving immune function, and improving the quality of life for individuals living with HIV/AIDS.
- Mechanism of Action of Antiretroviral Therapy:
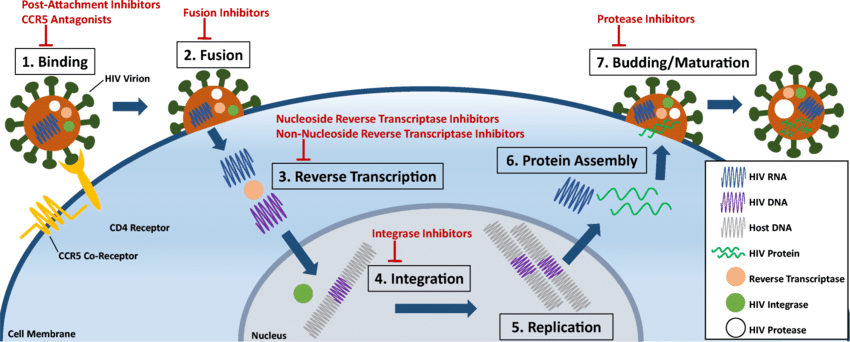
- Antiretroviral drugs target various stages of the HIV replication cycle, inhibiting viral entry into cells, reverse transcription of viral RNA into DNA, integration of viral DNA into the host genome, and viral assembly and release.
- By disrupting these processes, ART suppresses viral replication and reduces the viral load in the body.
- Components of Antiretroviral Therapy: ART typically consists of a combination of antiretroviral drugs from different classes, including:
- Nucleoside Reverse Transcriptase Inhibitors (NRTIs): These drugs interfere with the reverse transcription process, preventing the conversion of viral RNA into DNA. Examples include tenofovir, emtricitabine, and abacavir.
- Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs): NNRTIs bind to and inhibit the activity of the HIV reverse transcriptase enzyme, blocking viral replication. Examples include efavirenz, nevirapine, and rilpivirine.
- Protease Inhibitors (PIs): PIs block the activity of the HIV protease enzyme, preventing the cleavage of viral polyproteins and the maturation of infectious viral particles. Examples include ritonavir, atazanavir, and darunavir.
- Integrase Strand Transfer Inhibitors (INSTIs): INSTIs inhibit the integration of viral DNA into the host genome, preventing the establishment of a permanent viral reservoir. Examples include raltegravir, dolutegravir, and bictegravir.
- Entry Inhibitors: Entry inhibitors block the interaction between viral proteins and host cell receptors, preventing viral entry into cells. Examples include maraviroc and enfuvirtide.
- Benefits of Antiretroviral Therapy:
- Viral Suppression: ART reduces the viral load in the body, slowing disease progression and preserving immune function.
- Prevention of Opportunistic Infections: By restoring immune function, ART helps prevent opportunistic infections and AIDS-related complications.
- Improvement in Quality of Life: Effective ART allows individuals living with HIV/AIDS to lead healthier and more productive lives, reducing morbidity and mortality.
- Prevention of Transmission: Viral suppression achieved through ART significantly reduces the risk of HIV transmission to sexual partners and vertical transmission from mother to child during pregnancy and childbirth.
How has the ART Evolved in Ensuring Effective Treatment?
- Evolution:
- At the emergence of HIV/AIDS in the early 1980s, the disease was considered a death sentence and was met with a lot of fear, stigma and discrimination.
- While the US FDA approved the first antiretroviral drug, AZT (zidovudine), in March 1987, three additional drugs were approved in 1988. A new class of antiretroviral drugs, protease inhibitors, was introduced in 1995. However, access to these medicines remained limited for most of the world's population, except in some high-income countries.
- Global Efforts:
- Recognising this challenge, in 2000, at the UN General Assembly’s Millennium Summit, world leaders set a specific goal and issued the declaration to stop and reverse the spread of HIV.
- The Global Fund to Fight AIDS, Tuberculosis and Malaria was created in 2002 which advocated universal access to HIV prevention, treatment, care and support services.
- In 2004, the number of PLHIV in India was estimated to be 5.1 million, with a population prevalence of 0.4%. Very few of them were on antiretroviral therapy. Even by the end of 2004, only 7,000 PLHIV were on ART.
- Barriers to ART’s Evolution:
- The key barrier to ART was high cost and unaffordability for individuals, and geographical access to treatment.
- In fact, the so-called “cocktail therapy’ or HAART (highly active antiretroviral therapy), a combination of three or more anti-retroviral drugs, had become available starting in 1996, but costs were prohibitively high (USD 10,000 a year).
- People infected with HIV were stigmatised and lost their lives while health-care providers felt helpless due to non-availability/non affordability of ARTs.
- Necessity for Free Treatment:
- The decision to make free ART for any adult living with HIV was a path-breaking one. From November 2006, the free ART was made available for children as well.
- In two decades of free ART initiative, the facilities offering ART have expanded from less than 10 to around 700 ART centres - 1,264 Link ART centres have provided, and are providing, free ART drugs to approximately 1.8 million PLHIV on treatment.
- Effectiveness of ART:
- ART is not merely about starting a person living with HIV on treatment. It is equally important to keep the viral load down and suppressed to ensure that the transmission of diseases is also halted.
- The impact has been that in 2023, the prevalence of HIV in 15-49 years has come down to 0.20 (confidence interval 0.17%-0.25%) and the burden of disease in terms of estimated PLHIV has been coming down to 2.4 million.
- Usefulness for Indian Population:
- India’s share in PLHIV globally had come down to 6.3% (from around 10% two decades ago). As of the end of 2023, of all PLHIV, an estimated 82% knew their HIV status, 72% were on ART and 68% were virally suppressed.
- The annual new HIV infections in India have declined by 48% against the global average of 31% (the baseline year of 2010). The annual AIDS-related mortalities have declined by 82% against the global average of 47% (the baseline year of 2010).
What were the Factors that Made ART Intervention Successful?
- Patient-Centric Approach to Services:
- It will be unfair to credit free ART alone for the success. There were many complementary initiatives which have contributed to halting the HIV epidemic.
- These include the provision of free diagnostic facilities; attention on prevention of parent to child transmission of HIV (PPTCT) services; prevention, diagnosis and management of opportunistic infections including management of co-infections such as tuberculosis (TB).
- Incorporating Dynamic Modifications:
- The programme has shown agility and dynamic modifications. Early initiation of ART and Treat all policy evolved over the years where the ART eligibility criteria were relaxed - from those having a CD4 count less than 200 cells/mm3 (in 2004), to that less than 350 cells/mm3 (in 2011), and then to less than 500 cells/mm3 (in 2016).
- Promoting Universalization:
- There was the ‘Treat All’ approach from 2017, which ensures that ART is initiated, irrespective of CD4 count. This has been a true universalisation and has contributed to reduced virus transmission, both at the individual and the community levels.
- Note:
- The World Health Organization's (WHO) “Treat All” guidance of September 2015, recommended that all individuals be treated as soon as possible after HIV infection and diagnosis.
- In addition, because reduction in HIV viral load to undetectable levels eliminates the risk of onward transmission, the Treat All approach has the potential to provide the population health benefit of reducing HIV incidence.
- Affordable and Free ART:
- The programme also adopted a free of cost viral load testing for all PLHIV on treatment, by providing two to three months of medicines to stable PLHIV which minimises the number of patient visits to the ART centres, reducing travel time and costs for the patients.
- This approach also increases adherence to treatment besides decongesting ART centres by reducing the average daily OPD, giving health-care workers more time to attend to other patients.
- Adding New Medicines:
- India continued to add newer and more potent drugs to the programme, as and when those became available. For example, Dolutegravir (DTG), a new drug with superior virological efficacy and minimal adverse effects was introduced in 2020.
- In 2021, India adopted a policy of rapid ART initiation in which a person was started on ART within seven days of HIV diagnosis, and in some cases, even the same day.
Concerns in ART Treatment:
- First, the delayed enrolment to the ART facilities is the biggest challenge to the national programme. In India, patients presenting with CD4 count <200 to ART centres constitute almost a third of total foot fall.
- Second, after starting on ART and continuing, the patient starts feeling well. But the moment this happens, they start missing doses and miss medicines for months or completely drop out. This results in the development of resistance as well. This ‘loss to follow up’ needs to be addressed.
What are India's Efforts to Prevent HIV?
- HIV and AIDS (Prevention and Control) Act, 2017:
- According to this act, the central and state governments shall take measures to prevent the spread of HIV or AIDS.
- Access to ART:
- India has made Antiretroviral Therapy (ART) affordable and accessible to over 90 per cent of people living with HIV in the world.
- Memorandum of Understanding (MoU):
- The Ministry of Health and Family Welfare signed a MoU with the Ministry of Social Justice and Empowerment in 2019 for enhanced HIV/AIDS outreach and to reduce the incidence of social stigma and discrimination against victims of drug abuse and Children and People Living with HIV/AIDS.
- Project Sunrise:
- Project Sunrise was launched by the Ministry of Health and Family Welfare in 2016, to tackle the rising HIV prevalence in north-eastern states in India, especially among people injecting drugs.
What Steps Need to be Taken to Make ART Treatment More Effective?
- Ensuring Sustained Supply and Availability:
- The sustained supply and availability of ART needs to be ensured by the national programme, in every geography of the country and more so for tough terrain, hilly and remote areas.
- There is a need to focus on the private sector engagement in care of PLHIV, which can ensure efficient supply by deploying their expertise.
- Need for Constant Training:
- This ongoing evolution requires that staff stay updated with the latest advancements and techniques in their field. Moreover, training should emphasise hands-on learning to ensure that staff can effectively apply theoretical knowledge in practical situations.
- This approach not only enhances their skills but also improves their problem-solving abilities and adaptability to new challenges.
- Strengthening Integration with Other Programmes:
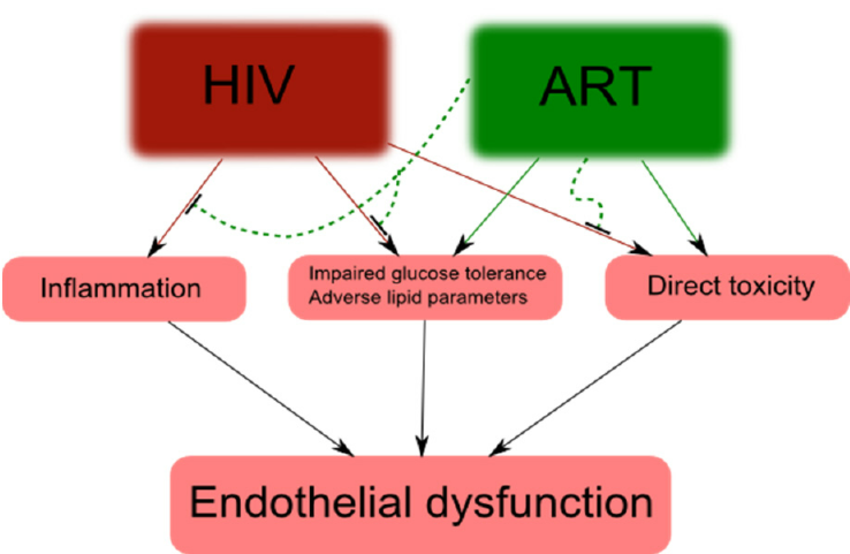
- There is a need to focus on strengthening integration with other programmes such as hepatitis, non-communicable diseases (diabetes and hypertension) and mental health as PLHIV are living normal but have other health conditions that need to be addressed.
- A focused approach needs to be adopted to reduce preventable mortality that includes systematic death reviews and availability of advanced diagnostics.
- Adopting a Multi-Sectoral Approach:
- The free ART initiative in India can be made more effective by ensuring the political will and constant support of successive governments; sustained and sufficient funding, regular programme reviews and field-based monitoring, a series of complementary initiatives; community and stakeholder engagements and participation; people-centric modifications in the service delivery; bridging the policy intentions to implementation gaps, and continuous expansion of services to cover more people living with HIV.
- Implementing National AIDS Control Programme (NACP):
- The ongoing and fifth phase of India’s National AIDS Control programme (NACP) aims to (by 2025) reduce the annual new HIV infections by 80%, reduce AIDS-related mortalities by 80% and eliminate vertical transmission of HIV and syphilis.
- To achieve this, NACP phase 5 calls for the attainment of ambitious targets of 95-95-95 by 2025, where 95% of all people living with HIV know their HIV status; 95% of all people diagnosed with HIV infection receive sustained antiretroviral therapy (ART), and 95% of all people receiving antiretroviral therapy achieve viral suppression by 2025. These targets are aligned with global targets agreed by the UNAIDS.
Conclusion
The free ART initiative arguably paved the path for bending the HIV/AIDS epidemic curve in India. It is a testament to the point that if there is a will, the government-run public health programme can deliver quality health services free, and available and accessible to everyone. The 20 years of free ART and subsequent steps under the NACP have the potential to guide other public health programmes in the country. As an example, the learnings can and should be used to launch a nationwide free Hepatitis C treatment initiative in India and accelerate progress towards Hepatitis C elimination.
|
Drishti Mains Question: Describe the challenges in providing Antiretroviral Therapy (ART) to HIV/AIDS patients in rural areas of India. Critically analyse the effectiveness of India's National AIDS Control Program in combating the HIV/AIDS epidemic. |
UPSC Civil Services Examination Previous Year Question (PYQ)
Q. Which of the following diseases can be transmitted from one person to another through tattooing? (2013)
- Chikungunya
- Hepatitis B
- HIV-AIDS
Select the correct answer using the codes given below:
(a) 1 only
(b) 2 and 3 only
(c) 1 and 3 only
(d) 1, 2 and 3
Ans: (b)